Are you noticing persistent bumps on your scalp and wondering if it’s just dandruff or something more? Seborrheic dermatitis and dandruff, while often discussed separately, are actually related conditions on a spectrum. Understanding the nuances between them is key to managing those bothersome bumps.
Quick highlights:
- Dandruff & Seborrheic Dermatitis are related: Think of dandruff as the milder scalp-specific version, and seborrheic dermatitis as more widespread and intense.
- Bumps are a key differentiator: Bumps are more common and prominent in seborrheic dermatitis due to inflammation.
- Malassezia yeast is the culprit: Overgrowth of this yeast plays a central role in both conditions.
- Treatment varies: Knowing which condition you’re dealing with is crucial for effective treatment.
This article breaks down the causes of bumps in both dandruff and seborrheic dermatitis, helping you distinguish between the two and understand your treatment options.
Seborrheic Dermatitis vs. Dandruff: What’s the Difference?
Seborrheic dermatitis and dandruff are not entirely separate entities but rather different expressions of the same underlying issue. Dandruff is generally considered a milder form, mainly affecting the scalp with flaking. Seborrheic dermatitis is the more severe and extensive form, causing inflammation, bumps, and affecting areas beyond just the scalp, such as the face and chest [1].
Let’s delve deeper into what each condition entails.
What are seborrheic dermatitis and dandruff?
Seborrheic dermatitis is a chronic inflammatory skin condition that commonly affects areas rich in oil glands (sebaceous glands). This includes the scalp, face, and chest [2]. Hallmark symptoms include skin flaking, redness, and the development of bumps.
Dandruff, on the other hand, is specifically characterized by mild scalp flaking without significant inflammation [2]. It’s often considered a less severe presentation confined to the scalp.
Interestingly, both conditions share a common link: an overgrowth of Malassezia yeast, a fungus that naturally resides on our skin [3]. Research indicates that Malassezia breaks down sebum (scalp oil) into fatty acids. These fatty acids can trigger an inflammatory response in susceptible individuals, leading to the flaking and bump formation characteristic of these conditions [5] [DOI: 10.1016/j.clindermatol.2020.10.013]. Furthermore, genetics and stress can influence sebum production, making some people more prone to experiencing flare-ups of seborrheic dermatitis or dandruff [4].
Bumps in Seborrheic Dermatitis: Unpacking the Causes
Bump development, specifically pustules and papules, is a key feature of seborrheic dermatitis. Microscopic examination reveals that inflammatory cells and serum accumulate between skin cells (keratinocytes), leading to the formation of intraepidermal pustules [5].
Several factors contribute to these bumps in seborrheic dermatitis:
- Malassezia Yeast Overgrowth: As mentioned, an excess of Malassezia yeast on the skin is strongly linked to seborrheic dermatitis [7]. This overgrowth triggers inflammation, resulting in the formation of papules and pustules [8][3].
- Inflammation: During a flare-up, the skin’s papillae (small nipple-like projections) become swollen (edematous). Blood vessels (capillaries) engorge and release serum and immune cells (leukocytes) into the epidermis [10][11]. This process damages keratinocytes and contributes to pustule formation.
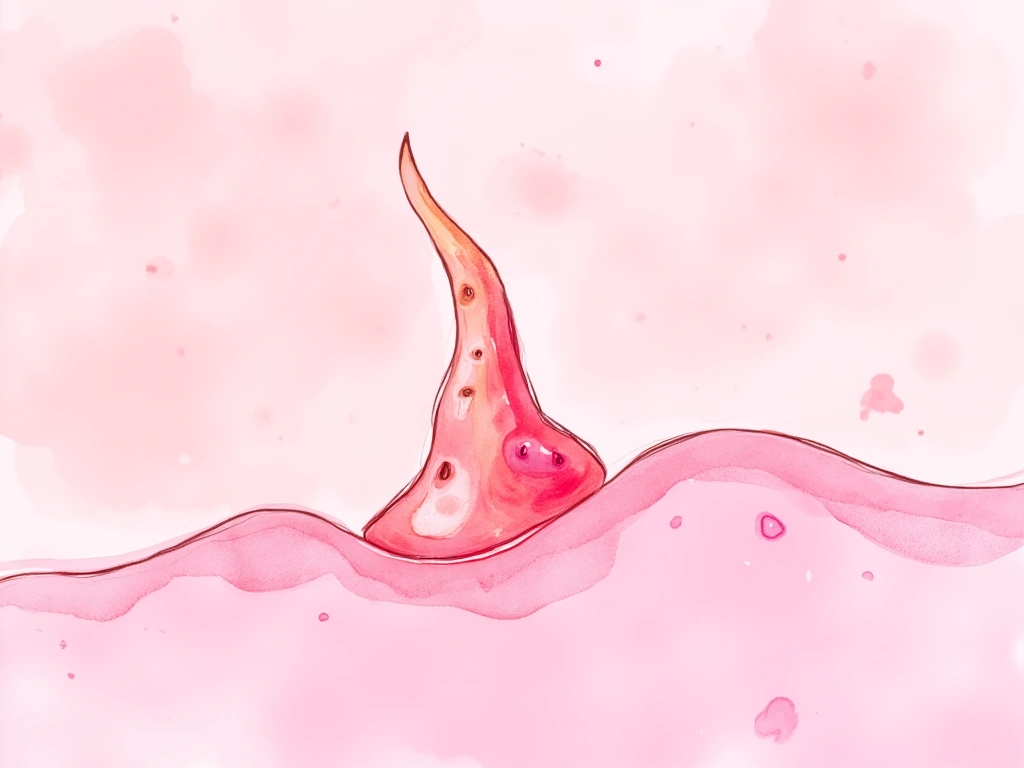
- Folliculitis: The yeast infection can extend into hair follicles, causing folliculitis, an inflammation of the hair follicles. This presents as papules [6]. Folliculitis is a common finding in seborrheic dermatitis [7].

Bumps in Dandruff: Why They Might Appear (Rarely)
While dandruff is primarily characterized by scaling without significant inflammation, bumps are not typical. However, in cases of severe dandruff with extensive scaling, bumps can sometimes occur due to secondary issues [4].
Here’s how bumps might develop in severe dandruff:
- Dry Flakes and Irritation: Excessively dry scalp flakes can cause itching and rubbing, potentially irritating sensitive skin and leading to papule formation.
- Secondary Bacterial Infection: Accumulated flakes can create an environment where bacteria, particularly Staphylococcus species, can colonize. This can lead to bacterial folliculitis, manifesting as papules or pustules [8]. It’s important to note that this is considered a secondary infection, not a primary feature of dandruff itself.
- Progression to Seborrheic Dermatitis: In some cases, a high Malassezia load might escalate a mild dandruff condition into full-blown seborrheic dermatitis, complete with the associated papules and pustules. However, typical mild dandruff usually doesn’t involve Malassezia levels high enough to cause significant inflammation.
It’s crucial to remember that papules are not a hallmark of dandruff, which lacks a true inflammatory component [4, 2]. Bumps in dandruff are usually a sign of a complication or a condition that may be progressing towards seborrheic dermatitis.
In short: Bumps are not typical in dandruff. If bumps are present, consider secondary effects or progression to seborrheic dermatitis.

Common Triggers for Bumps in Both Conditions
Several factors can trigger or worsen bump formation in both seborrheic dermatitis and, less commonly, in severe dandruff:
- Genetic Predisposition: A family history of these conditions increases your susceptibility.
- Sebum Overproduction: Excess scalp oil provides a rich environment for Malassezia yeast to thrive.
- Environmental Factors: High humidity, sweating, and occlusive hair products can exacerbate yeast overgrowth and inflammation.
- Immune Response: An overreactive immune system can exaggerate the inflammatory response to Malassezia [6].
Folliculitis: A Closer Look at Hair Follicle Inflammation
Folliculitis, or inflammation of hair follicles, is frequently seen in seborrheic dermatitis. Yeasts and skin oils can clog hair follicles [puddy doi-“10.1016/j.clindermatol.2020.10.013”], leading to red, sometimes painful or itchy papules around hair shafts [17]. Pustules may also form around the hair follicles.
Untreated folliculitis can have consequences like hair loss and scarring. In severe cases, systemic symptoms such as fever are possible [8]. Recognizing the various ways folliculitis can present is important for proper management.
Factors that increase your chances of developing folliculitis include:
- Younger age
- Family history of folliculitis
- Excessive sweating
- Use of oily or greasy hair products [8][9]
Environments like swimming pools and hot tubs can also increase the risk of complications from folliculitis [8].

Rule Out Other Culprits: Similar Conditions to Consider
It’s important to remember that other skin conditions can mimic seborrheic dermatitis and dandruff bumps. These include:
- Psoriasis: Scalp psoriasis can cause raised, red plaques with silvery scales and bumpy, flaky patches [10].
- Bacterial Folliculitis: A Staphylococcus bacterial infection of the hair follicles causes pustules [8].
- Fungal Infections (Ringworm): Scalp ringworm presents as a red, ring-shaped rash and can cause hair loss [11].
- Allergic Reactions: Contact dermatitis from hair products can cause itchy, red bumps [12].
Given the overlap in symptoms, consulting a dermatologist for an accurate diagnosis is crucial when scalp bumps appear. A professional evaluation ensures you receive the most appropriate treatment.

Treatment Strategies: Getting Rid of Bumps
Treatment approaches are tailored to the specific diagnosis.
- Over-the-counter (OTC) Antifungal Shampoos: Shampoos containing zinc pyrithione or ketoconazole are effective in reducing Malassezia yeast levels for both seborrheic dermatitis and dandruff [3][13].
- Topical Steroids: These are used to reduce inflammation and address folliculitis papules associated with seborrheic dermatitis flare-ups [4].
- Oral Antifungal Medications: For severe, widespread, or treatment-resistant seborrheic dermatitis, oral antifungals like fluconazole or itraconazole may be prescribed for 2-4 weeks [DOI:10.1159/000442763].
A word of caution on topical steroids: While effective for inflammation, long-term, unsupervised use of topical steroids can lead to side effects.
Identifying if seborrheic folliculitis is present alongside seborrheic dermatitis will guide the selection of appropriate anti-inflammatory and antimicrobial treatments [].

Key Takeaways: Managing Scalp Bumps
In conclusion, while both seborrheic dermatitis and dandruff involve Malassezia overgrowth, their presentation and the causes of bumps differ. Seborrheic dermatitis is characterized by inflammation-driven bumps, often linked to folliculitis, while bumps in dandruff are less common and usually secondary to irritation or infection.
Key Insights Recap:
- Distinguish Between Conditions: Recognizing the differences between dandruff and seborrheic dermatitis is the first step to effective management.
- Understand Triggers: Genetics, sebum production, environment, and immune response play a role in bump formation.
- Folliculitis Matters: Folliculitis is a significant factor in seborrheic dermatitis bumps and requires appropriate treatment to prevent complications.
Important Considerations:
- Don’t Self-Diagnose: Scalp bumps can have various causes. Rule out other conditions like psoriasis or bacterial infections.
- Seek Professional Help: A dermatologist can provide an accurate diagnosis and personalized treatment plan.
Treatment Options Summary:
- OTC Antifungal Shampoos: A good starting point for managing yeast overgrowth.
- Topical Steroids (with caution): Effective for inflammation in seborrheic dermatitis.
- Oral Antifungals (for severe cases): May be necessary for resistant seborrheic dermatitis.
Ultimately, if you’re experiencing bumps on your scalp, understanding whether it’s dandruff, seborrheic dermatitis, or another condition is crucial. Consulting a dermatologist is the best way to get to the root of the problem and receive targeted, effective treatment.
No Comments
Be the first to start a conversation