- Seborrheic dermatitis is a common skin condition affecting millions.
- This article explores the potential link between vitamin D levels and seborrheic dermatitis.
- We review existing medical studies and online discussions to understand this connection.
- While research is limited, ensuring adequate vitamin D is crucial for overall skin and general health.
- If you have seborrheic dermatitis, testing your vitamin D levels might be beneficial.
This article attempts to decipher the potential role of vitamin D in seborrheic dermatitis progression. We will focus on answering these key questions:
- Can vitamin D deficiency contribute to seborrheic dermatitis?
- Can vitamin D supplementation help alleviate symptoms?
- What is vitamin D’s role in maintaining healthy skin?
We’ll begin with a brief overview of seborrheic dermatitis, then examine the evidence for vitamin D’s potential involvement, and conclude by highlighting the broader importance of vitamin D for your health.
We hope you find this article insightful! If any questions arise or you’d like to discuss these topics further, please use the [contact form][1] at the bottom of this page.
Seborrheic Dermatitis: A Quick Overview
Seborrheic dermatitis has been discussed in detail in other sections of this website, particularly in this comprehensive .
However, if you’re looking for a quick refresher or already know the basics, here’s a summary of the key characteristics of seborrheic dermatitis:
- Affects approximately 3% of adults.
- More prevalent in individuals with HIV or Parkinson’s disease.
- Symptoms include skin flaking, inflammation, itching, and imbalanced sebum production (both dry and oily types).
- Scalp is the most commonly affected area; mild cases are known as dandruff.
- Facial areas frequently impacted: nose, cheeks, forehead, ears, and eyebrows.
- Can also appear on other sebum-rich areas like the lower back and chest.
- Malassezia yeast is often implicated, but broader skin flora imbalances may be more significant.
- Oleic acid, a byproduct of skin microflora, is thought to contribute to symptoms.
- Common treatments include topical antifungals and corticosteroids, as well as lithium salts and other medications.
- Currently, there is no known cure, and ongoing management is usually recommended to maintain remission.
In essence, the exact mechanisms behind seborrheic dermatitis remain unclear. While treatments often provide relief, many sufferers experience unpredictable flare-ups and may find their symptoms become resistant to standard treatments over time.
For those seeking long-term solutions beyond continuous treatment, understanding potential contributing factors like vitamin D is crucial.

Vitamin D and Seborrheic Dermatitis: Is There a Connection?
Anecdotal reports online suggest some individuals have found relief from seborrheic dermatitis through vitamin D supplements or increased sun exposure. However, the scientific evidence supporting this is limited, and formal research on vitamin D as a treatment for seborrheic dermatitis is scarce.
To determine if pursuing vitamin D supplementation is a worthwhile avenue, we need to separate anecdotal claims from scientific evidence. Let’s examine the existing medical literature to see what insights it offers.
Examining the Medical Research
A search of academic databases reveals a few studies that touch upon the topic of vitamin D and seborrheic dermatitis. Here’s a summary of the relevant findings:
Nutrient Mediators in Psoriasis and Seborrheic Dermatitis (1988) [1]
- This older paper briefly mentions a successful case of vitamin D3 in treating psoriasis [].
- It does not discuss vitamin D’s use in seborrheic dermatitis.
- The paper notes the increasing use of PUVA therapy (psoralen and UVA exposure) for skin disorders, highlighting its immune-suppressing effects.
Takeaway: This early study doesn’t directly address vitamin D and seborrheic dermatitis, but it hints at vitamin D’s potential role in skin conditions and the use of UV light (which stimulates vitamin D production) in dermatology.
Vitamin D Supplementation and Seborrheic Dermatitis Recurrences (2017) [2]
- This study investigated vitamin D supplementation in 36 people with seborrheic dermatitis.
- Participants received 1600 IU of cholecalciferol (vitamin D3) daily for 3 months during fall/winter to minimize sun exposure.
- All participants were vitamin D deficient at the start, with levels below 21ng/l.
- The study relied on patient self-reports of flare-up frequency and severity.
- Results: 65.5% reported fewer recurrences, 22% no change, and 12.5% reported worsened symptoms.
- The authors observed that individuals with the lowest initial vitamin D levels seemed to experience the most benefit from supplementation.
Takeaway: This study suggests a potential benefit of vitamin D supplementation for reducing seborrheic dermatitis flare-ups, particularly in vitamin D deficient individuals. However, it’s based on self-reported data and a relatively small sample size.
Vitamin D Levels in Seborrheic Dermatitis Patients (2013) []
- From the same author as the 2017 study, this paper assessed 25-hydroxyvitamin D levels in 22 seborrheic dermatitis patients.
- Vitamin D levels were categorized as:
- 29-21 ng/mL (insufficiency): 4 individuals
- 20-10 ng/mL (deficiency): 13 individuals
- Below 10 ng/mL (severe deficiency): 2 females
- The authors noted that levels below 30ng/mL are generally considered insufficient, below 20ng/mL deficient, and below 10ng/mL severely deficient.
- The study was motivated by the increasing use of vitamin D analogs in psoriasis treatment and vitamin D’s known role in immune regulation.
Takeaway: This study indicates that vitamin D deficiency and insufficiency may be common in people with seborrheic dermatitis, supporting the idea of a potential link.
Vitamin D Deficiency in the General Population
In the United States, it is estimated that 6-8% of the general adult population has vitamin D deficiency (below 30ng/mL) [4].
Topical Vitamin D in Dermatology: A Review (2014) [5]
- This review examined the use of topical vitamin D analogs for various skin conditions.
- Mechanism of Action: Topical vitamin D analogs regulate calcium balance and affect vitamin D receptors in the skin. These receptors influence skin cell (keratinocyte) production, immune cell (T-cell) regulation, and cytokine levels.
- Early small studies showed promise for topical vitamin D analogs in seborrheic dermatitis [6].
- However, larger, randomized controlled trials yielded contradictory results.
- Conclusion: The review authors do not recommend topical vitamin D analogs for treating facial or scalp seborrheic dermatitis.
Takeaway: Research on topical vitamin D for seborrheic dermatitis is inconclusive, with larger studies favoring traditional treatments like corticosteroids. This review focuses on topical applications, not oral supplementation.
Overall Medical Literature Review Summary: The limited research on vitamin D and seborrheic dermatitis is mixed. Studies by Dimitrova suggest a possible link between vitamin D deficiency and seborrheic dermatitis and hint at benefits from supplementation. However, research on topical vitamin D analogs has not shown them to be effective for seborrheic dermatitis. More robust research is needed to draw firm conclusions.
Insights from Online Discussions
Beyond medical journals, let’s explore what people are saying online about vitamin D and seborrheic dermatitis.
- Reddit – Negative Experiences: Some Reddit users [reddit][2] report that vitamin D supplementation did not help their seborrheic dermatitis.
- One user took 10,000 IU of vitamin D daily for a year with no improvement.
- Others suggest digestive issues and nutrient absorption problems might be more relevant for many sufferers.
- Reddit – Positive Experience (with Zinc): Another Reddit user [user from reddit][3] credits vitamin D and zinc supplements for helping manage their seborrheic dermatitis.
-
CureZone Forum – Positive Experience (with other supplements): An older post on CureZone [forum participant over at CureZone][4] mentions vitamin D, calcium, and caprylic acid as helpful supplements, with kefir (a probiotic food) being highlighted as most beneficial.
Takeaway from Online Discussions: Online experiences are varied. Some individuals report no benefit from vitamin D supplementation, while others suggest it may be helpful, sometimes in combination with other supplements or dietary changes. These are anecdotal accounts and not scientific evidence.
Vitamin D and Seborrheic Dermatitis: Is Vitamin D a Viable Treatment?
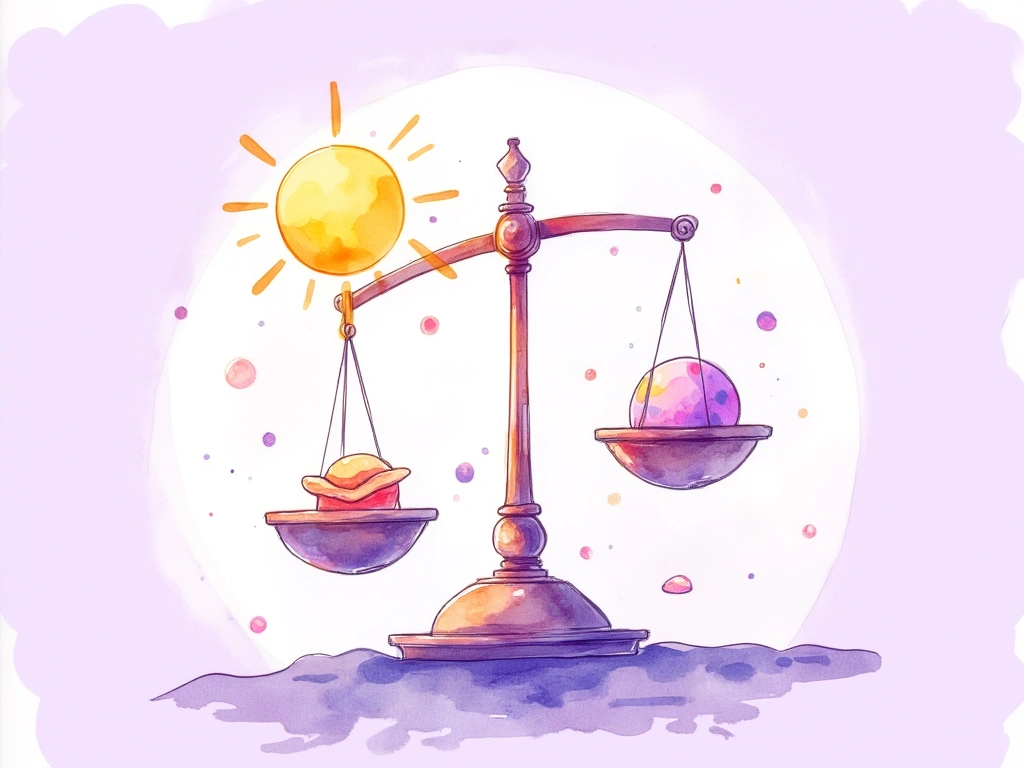
Based on the evidence we’ve reviewed, vitamin D does not appear to be a definitive or consistently effective treatment for seborrheic dermatitis. Neither vitamin D supplements nor topical vitamin D analogs have strong empirical support, and even anecdotal reports are inconsistent.
However, the research does suggest that lower vitamin D levels might be common in individuals with seborrheic dermatitis. Therefore, if you have seborrheic dermatitis, it’s prudent to have your vitamin D levels checked by a doctor to rule out deficiency and address any broader health risks associated with low vitamin D.
Why Vitamin D Matters: Beyond Skin Health
The importance of vitamin D often goes underestimated, but maintaining adequate levels is crucial for overall well-being.
Vitamin D deficiency has been linked to an increased risk of autoimmune diseases, cancer, bone problems, and cardiovascular disease [22]. Ensuring sufficient vitamin D throughout life is therefore essential for overall health maintenance.
Vitamin D is a broad topic beyond the scope of this article, but abundant information is available online. A helpful starting point is this comprehensive review paper from 2005:
[Benefits and requirements of vitamin D for optimal health: a review.][5]
Vitamin D’s Specific Role in Skin Health
Humans primarily synthesize vitamin D in the skin through UV exposure (approximately 80%) [], with the remainder coming from dietary sources. This highlights vitamin D’s intrinsic link to skin physiology. Even without a definitive link to seborrheic dermatitis treatment, understanding vitamin D’s role in skin health is valuable.
Vitamin D and its receptors play several key roles in skin health:
- Regulating Skin Cell Growth: Vitamin D regulates the growth and differentiation of various skin cell types, including keratinocytes, the primary cells of the epidermis [23].
- Maintaining Skin Barrier Function: It influences the production of long-chain glycosylceramides, which are essential for a stable and effective skin barrier [24].
- Modulating Innate Immunity: Vitamin D helps stabilize the skin’s innate immune response, potentially preventing overreactions and autoimmune processes [25, 26, 27, 28].
- Supporting Regulatory T Cells: It increases the availability of regulatory T cells (Tregs), which are crucial for immune balance and preventing excessive inflammation [29, 30].
- Producing Antimicrobial Peptides: Vitamin D regulates the production of antimicrobial peptides, which help defend against pathogens [31, 32, 33].
- Protecting Against UV Damage: Vitamin D offers some protection against damage from ultraviolet (UV) radiation [34, 35, 36].
Skin’s Immune Response & Vitamin D Production
Interestingly, the skin’s immune system can locally influence vitamin D production. Monocytes, key immune cells in the skin, can promote localized activation of vitamin D when encountering microbial threats [37, 38].
Collectively, these functions underscore the importance of maintaining adequate vitamin D levels for overall skin health, and emphasize the potential benefits of stimulating vitamin D production in the skin through safe sun exposure when possible.
In Conclusion: Vitamin D and Seborrheic Dermatitis
This article has explored the potential relationship between seborrheic dermatitis and vitamin D, summarizing available evidence and online discussions. Here are the key takeaways:
1. The underlying cause of seborrheic dermatitis is not fully understood, though Malassezia yeast is a primary focus in medical research.
2. Online speculation exists regarding vitamin D’s role in seborrheic dermatitis, with some suggesting deficiency may worsen the condition and supplementation could provide relief.
3. Limited research indicates that vitamin D deficiency may be common among individuals with seborrheic dermatitis.
4. One small study showed some benefit from vitamin D supplementation in reducing flare-ups, but some participants reported worsening symptoms, and complete remission was not observed.
5. Anecdotal success stories are scattered online, but most online accounts do not report significant benefits from vitamin D alone.
6. Regardless of its direct impact on seborrheic dermatitis, adequate vitamin D is vital for general skin health, immune system balance, and chronic disease prevention.
7. If you have seborrheic dermatitis, it’s advisable to check your vitamin D levels and address any deficiency, with safe sun exposure being a recommended approach to boost vitamin D production.
We hope this examination of the complex relationship between seborrheic dermatitis and vitamin D has been helpful. If you have questions, insights to share, personal experiences, or anything else to contribute, please drop a comment below.
I’ve had issues with s. dermatitis for the last 3 years or so strictly on my scalp. Recently, I switched to a multivitamin with a higher dose of vitamin D (1600 IU, actually the dose referenced in the one of the studies above) and after about three months of daily use my scalp is about 85% improved! Still occasional itchiness but no more scabs and inflammation. It’s completely clear. Can I prove it’s the vitamin D which is causing the improvement? Of course not. But in the process of trying to figure out what I was doing differently I remembered the change in multivitamin and googled about vitamin d and s. dermatitis and I’m intrigued by what I’ve found. Could be worth looking for sufferers as 1600 IU is a very modest dose of vitamin D. Good luck!
UV rays are effective to treat seborrheic dermatitis.
Maybe vitamin D deficiency and seborrheic dermatitis are not causally linked. Maybe it is just that people who don’t receive enough sunlight, get affected by both. Both get worse in winter.
Maybe its is vitamin K2. Or a combination of Vitamin D3 and K2. There is a study about atopy and k2 from Tokyo but in kids.