- Itchy, flaky eyelids? Seborrheic blepharitis is likely the culprit.
- More than just ‘eye dandruff’: Understand the distinct symptoms and why it needs proper care.
- Gentle yet effective treatments: Learn how to soothe and manage flare-ups around your sensitive eyes.
- Long-term management: Discover tips to reduce recurrences and maintain healthy eyelids.
Seborrheic dermatitis on the eyelids, or seborrheic blepharitis, can be persistent and uncomfortable. While it’s related to seborrheic dermatitis elsewhere on the body, treating it around the eyes requires extra care. This article will guide you through understanding and managing this condition effectively.
What you will learn:
- Key differences between eyelid skin conditions.
- Defining features and symptoms of seborrheic blepharitis.
- The importance of timely treatment for eye health.
- Effective treatment approaches for eyelids.
- Practical tips to minimize flare-ups.
Let’s explore how to address seborrheic blepharitis and find relief. If questions arise as you read, [join the discussion][1] in the comments.
Understanding Seborrheic Dermatitis: A Quick Overview
Seborrheic dermatitis is a common inflammatory skin condition, affecting roughly 3% of the population. It’s not completely understood, and a one-size-fits-all treatment doesn’t exist.
Key aspects of seborrheic dermatitis:
- It’s an inflammatory condition linked to sebaceous glands and sebum production.
- Malassezia yeasts are frequently implicated in symptom development.
- The prevailing theory suggests Malassezia yeasts break down sebum lipids, creating byproducts that trigger symptoms.
- Antifungal topicals are the standard medical treatment, targeting Malassezia and reducing symptom-causing byproducts.
Sebum is crucial in the cycle of seborrheic dermatitis, providing Malassezia yeasts with the lipids they need to produce irritating byproducts.
While eyelids lack sebaceous glands, they contain meibomian glands. These glands produce meibum, a lipid-rich sebum-like substance. This means eyelids have a lipid source for Malassezia, making them susceptible to seborrheic dermatitis.

Seborrheic Blepharitis or ‘Eyelash Dandruff’? Understanding the Terms
Dandruff is typically defined as a scalp condition characterized by itching, flaking, and dryness. This scalp-specific definition makes “eyelash dandruff” technically inaccurate.
Seborrheic Dermatitis of the Eyelids vs. Eyelash Dandruff
“Seborrheic dermatitis” and “dandruff” are often used interchangeably, causing confusion. While opinions vary, many experts consider dandruff a milder form of seborrheic dermatitis with less inflammation.
“Dermatitis” is a broad medical term for “skin inflammation.” “Seborrheic dermatitis” specifies inflammation related to sebaceous glands. However, for eyelids, “seborrheic blepharitis” is the most precise term.
“Blepharitis” medically means “eyelid inflammation.” Therefore, seborrheic dermatitis on the eyelids is accurately termed seborrheic blepharitis.
While these distinctions might seem technical, understanding them is key to correctly identifying and addressing seborrheic blepharitis.
Understanding the Four Main Types of Blepharitis
Like dermatitis, blepharitis presents in different forms. The four most common types [1] are:
- Staphylococcal blepharitis
- Seborrheic blepharitis
- Posterior blepharitis (Meibomian gland dysfunction)
- Demodex blepharitis
While overlap can occur, individuals usually experience one primary type of blepharitis.
Identifying Seborrheic Blepharitis: Key Symptoms
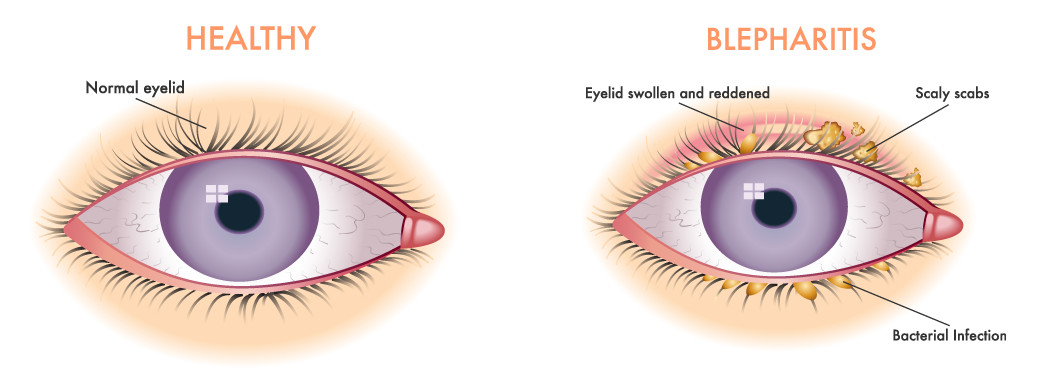
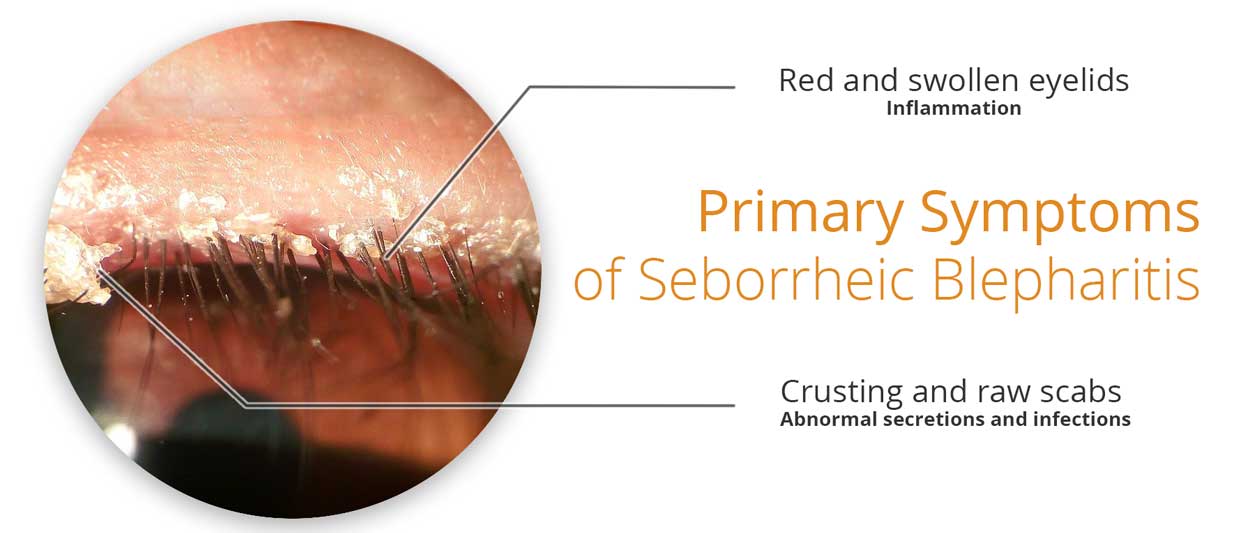
Compared to other blepharitis types, seborrheic blepharitis is characterized by these main symptoms [2, 1]:
- Greasy eyelid and eyelash crusting: Crusting is oily rather than dry.
- Significant inflammation: Noticeable redness and swelling.
- Co-occurring seborrheic dermatitis: Presence of seborrheic dermatitis on other skin areas.
A crucial indicator is the link to general seborrheic dermatitis. If you have seborrheic dermatitis on your face, scalp (dandruff), or chest and are experiencing eyelid issues, seborrheic blepharitis is highly probable.
Why Prompt Treatment for Seborrheic Blepharitis Matters
Seborrheic blepharitis can obstruct meibomian glands, reducing vital eyelid secretions. These secretions are critical for eye health. Untreated, prolonged blepharitis can lead to ocular surface damage and potential vision problems. One study reported corneal erosions in about 15% of seborrheic blepharitis patients [3].
Blepharitis is often chronic, lacking a single definitive cure. Management typically involves ongoing treatment to lessen symptoms and improve eyelid secretions.
Starting treatment early can significantly minimize the risk of complications.

Treatment Challenges and Considerations for Eyelids
The eyelids’ proximity to the eye and cornea’s sensitivity makes treatment delicate. While harsher treatments like tea tree oil or astringents might be used on other skin, they can severely irritate eyelids, causing more harm than good.
Considering the sensitivity of the eyelid area is crucial when choosing treatments.
Substances to generally avoid on eyelids include:
- Fragrances and volatile oils (essential oils): Despite tea tree oil’s success in some Demodex blepharitis cases [4, 5], they can be irritating.
- Strong acids or highly alkaline solutions: Can disrupt the delicate pH balance.
- Non-prescribed antifungals or antibiotics: Use only as directed by a doctor.
- Coal tar or tar-based products: Too harsh for eyelid skin.
- Sulfur preparations: Can be irritating in this area.
Individual tolerance varies, so this list is a general guide, not a strict rulebook.
Key Factors in Seborrheic Blepharitis
Understanding the processes involved in seborrheic blepharitis is important for effective treatment.
Based on research [6, 1], these factors are central to seborrheic blepharitis:
- Abnormal lid margin secretions: Altered quality and flow of meibum.
- Changes in lid margin microbes: Imbalance of bacteria and/or fungi.
- Dysfunctional tear film: Disruption of the eye’s protective tear layer.
- Increased inflammation: Inflammation of meibomian glands and eyelash follicles.
Altered secretions encourage microbial imbalance, further changing secretion composition. This reduces lipid content needed for tear film moisture, leading to dryness and itch.
These factors create a self-perpetuating cycle that can be difficult to break.

Six Treatment Approaches for Seborrheic Blepharitis
Medical literature commonly suggests these methods [6]:
- Warm Compresses: Restore normal secretions and soften crusts.
- Eyelid Cleansing: Remove buildup and promote healthy secretions.
- Antibiotics and Antifungals: Rebalance microbes and reduce colonization.
- Steroids: Reduce inflammation for symptom control (short-term use advised).
- Calcineurin Inhibitors: Modulate immune response and reduce inflammation cycle.
- Omega-3 Supplements: Reduce inflammation and potentially improve secretion quality (long-term approach).
Emerging treatments using heat and pulsed light to improve eyelid secretions are being explored [9], but are not yet standard practice.
Always Start with a Professional Diagnosis
Consulting a doctor is essential. Accurate diagnosis of your blepharitis type is the most critical step in effective treatment.
1. Warm Eyelid Compresses
Warm compresses, applied with a cotton pad or swab, are a standard first-line treatment.
How to apply warm compresses [1]:
- Boil water and let it cool to a comfortably warm temperature.
- Soak a clean cotton pad or washcloth in the warm water.
- Apply to the closed eye for 5-10 minutes, using a fresh pad/cloth each time.
- Repeat multiple times daily, spacing applications out.

Warm compresses aim to loosen crusts and promote normal secretions. While helpful, symptoms often return without further treatment.
Eyelid Massage: A Gentle Addition
Eyelid massage after warm compresses is often recommended, primarily for relieving associated eye symptoms, not directly improving blepharitis itself. Avoid excessive massage, as it can cause irritation and worsen symptoms [1].
2. Regular Eyelid and Eyelash Hygiene
Beyond warm compresses, specialized eyelid cleansers are available, designed to be gentle. However, no single solution is universally recommended. A simple, widely accepted cleansing method is saline solution.
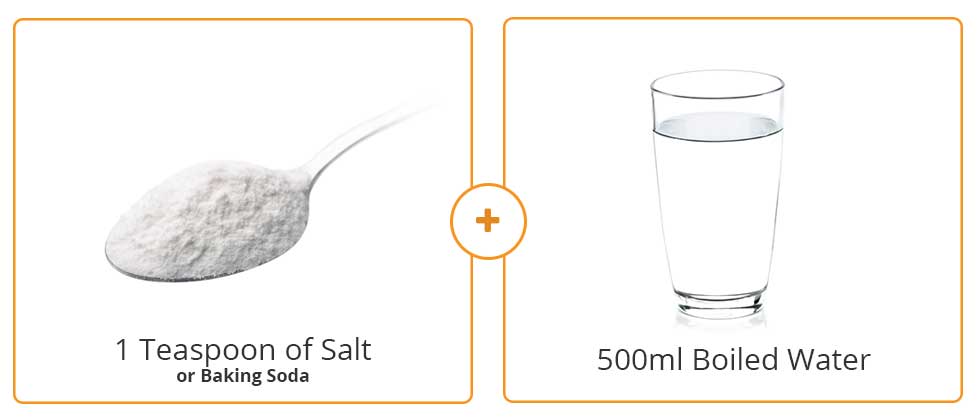
Saline eyelid cleansing [10]:
- Dissolve a heaped teaspoon of salt or sodium bicarbonate in 500ml of boiled water.
- Cool to a comfortable temperature.
- Use clean cotton swabs or pads to gently clean eyelids and eyelashes, discarding each after use.
For more detailed instructions, see:
[Community Eye Health – How to Clean Eyelids][2]
Baby Shampoo: Use with Caution
Some studies suggest diluted baby shampoo for eyelid cleaning [11, 8]. However, baby shampoos often have a low pH, which some experts consider detrimental to skin barrier function [12]. Use with caution and consider alternatives.
3. Antibiotics and Antifungals
Addressing microbial/fungal imbalance directly with antimicrobials or antifungals is often effective for blepharitis.
This treatment category often provides faster results. Due to the variety of available options, consult your doctor for the most appropriate treatment for your specific condition.
4. Topical Corticosteroids
Mild corticosteroid solutions (like hydrocortisone or dexamethasone) are frequently prescribed for blepharitis, including seborrheic blepharitis [13]. They reduce inflammation, providing rapid symptom relief.
However, steroid use on eyelids has risks. Steroids can thin the skin (atrophy), a concern on the already thin eyelid skin.
Other potential complications include:
- Increased eye pressure (intraocular pressure)
- Corneal and lens changes
Due to these risks, corticosteroid use around the eyes requires close medical supervision and should be short-term. Always consult a doctor before using corticosteroids for eyelid issues.
5. Calcineurin Inhibitors
Calcineurin inhibitors block calcineurin, a key chemical in skin inflammation.
Like steroids, they reduce inflammation and symptoms, allowing eyelid secretions to normalize.
Common calcineurin inhibitors include:
- Tacrolimus ointment
- Pimecrolimus cream
They generally have fewer steroid-related side effects like skin thinning or increased eye pressure [14].
However, calcineurin inhibitors still require a prescription and medical evaluation due to potential side effects [15]. Consult your doctor to see if they are suitable for you.
6. Omega-3 Supplementation
Omega-3 fatty acids are known to reduce systemic inflammation and improve immune function [16].
Studies on chronic blepharitis show promising results with omega-3 supplementation. A year-long study showed these improvements [8]:
- Improved eyelid secretion composition (in some participants)
- Reduced eyelid inflammation and symptoms (in some participants)
- Increased blood omega-3 levels
- Improved omega-3 to omega-6 fatty acid ratio
However, the long time frame for results, small study sizes, and incomplete understanding of secretion changes mean more research is needed.
Nonetheless, omega fatty acid balance is crucial for overall health, particularly for inflammatory conditions like seborrheic dermatitis.
Long-Term Care for Chronic Conditions
For chronic, relapsing conditions, addressing the immune system is key. Long-term strategies are generally more effective than quick fixes.
Additional Tips for Managing Seborrheic Blepharitis
These tips can support treatment and improve long-term outcomes:
- Avoid cosmetics during flare-ups: They can worsen inflammation and hinder healing.
- Use disposable applicators: Discard cotton swabs/pads after each use to prevent recontamination.
- Be cautious with home remedies: Online suggestions may introduce irritants and worsen symptoms.
- Treat seborrheic dermatitis elsewhere: Managing seborrheic dermatitis on other areas of the body can indirectly improve eyelid symptoms.
- Consider Demodex mites: Demodex infestation can mimic seborrheic blepharitis but requires different treatment and is often linked to rosacea, not seborrheic dermatitis [1].
This advice may be updated based on new information and user feedback in the comments.

In Summary: Managing Seborrheic Blepharitis
This article has provided a detailed overview of seborrheic blepharitis (seborrheic dermatitis of the eyelids, eyelash dandruff) and discussed various treatment options.
Key takeaways:
- “Seborrheic blepharitis” is the accurate term for seborrheic dermatitis affecting eyelids, with unique characteristics.
- Several blepharitis types exist with similar symptoms; accurate diagnosis is crucial.
- Seborrheic blepharitis symptoms include greasy crusting, inflammation, and co-existing seborrheic dermatitis elsewhere.
- Prompt treatment is recommended to prevent potential eye health issues.
- Eyelid skin sensitivity limits treatment options like strong topicals or corticosteroids.
- Removing buildup and managing microbial/fungal activity are key treatment goals.
- Consulting a doctor is highly recommended due to varied potential microorganisms involved.
- Long-term management with omega-3s and eyelid hygiene can reduce flare-up frequency and severity.
Share your experiences, suggestions, or questions in the comments below to continue the discussion.
We hope this information on managing seborrheic blepharitis (seborrheic dermatitis of the eyelids, eyelash dandruff) is helpful and relevant to you.

Loved it.
Very honest content.
Using Calcineurin suppressor drugs is not as better as steroids, yeah but for short period of span.
I suffer from seborratic derramities on the eyelids it is very painful. What can I do for seborrheic blephartis
I’m having Seborrheic dermatitis (scaly skin patch) on the corner of my eyelid close to the very top of my nose and right below my eyebrow. I had it in the past but it disappeared on its own. But this time it’s been a week. Any comments?