- Evidence-Based Approach: Ditch anecdotal advice and explore a diet for seborrheic dermatitis rooted in medical literature.
- Key Dietary Factors: Understand the crucial role of essential fatty acids, antioxidants, and gut health in managing seborrheic dermatitis.
- Actionable Plan: Get a practical, step-by-step dietary strategy to implement for potential symptom relief.
- Address Food Sensitivities: Learn how to identify and address potential food triggers through journaling and medical testing.
- Lifestyle Integration: Discover supplementary lifestyle changes to enhance your dietary approach and overall well-being.
This article attempts to determine the optimal diet for seborrheic dermatitis by moving beyond online forum advice and focusing on what medical literature suggests. We’ll evaluate research, understand the principles behind different dietary approaches, and develop an action-based plan to help you take control of your skin health from the inside out.
While navigating the often-sparse scientific data, we’ll stick to reputable sources and critical thinking. Your thoughts and experiences are welcome in the [comments section][1].
Thank you for reading, and I hope this article provides valuable insights for you.
Debunking Common Online Diet Advice for Seborrheic Dermatitis
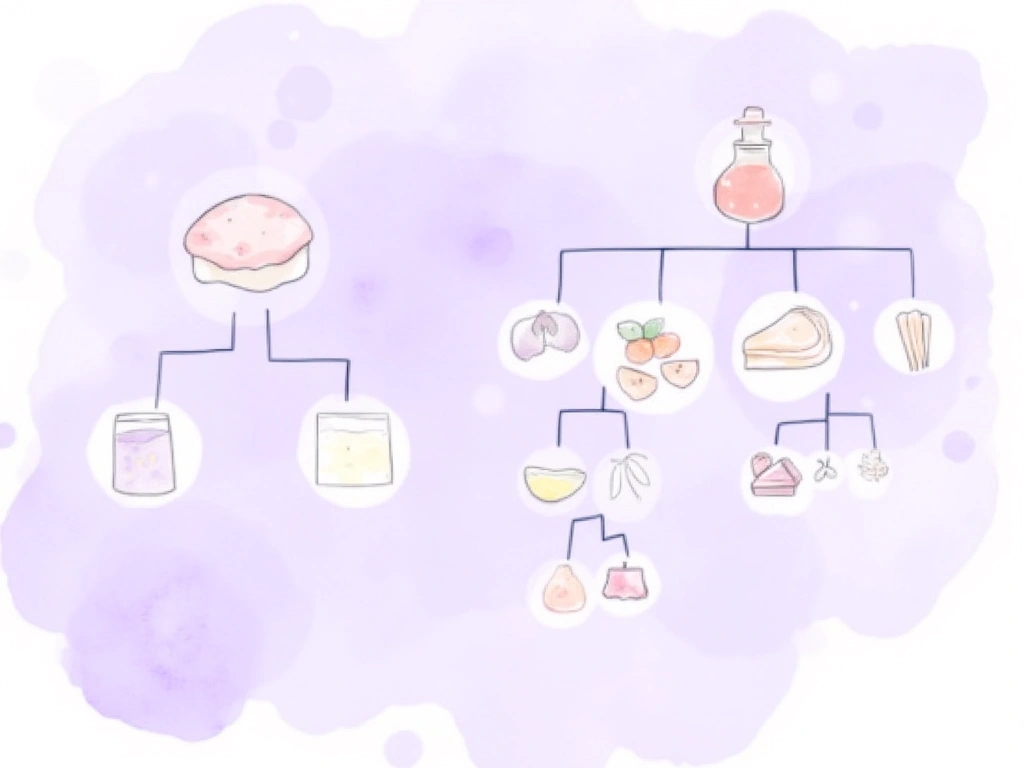
Searching online for seborrheic dermatitis diet advice often leads to a confusing mix of recommendations. The most frequently suggested dietary changes include:
- Avoid:
- Dairy
- Gluten
- Nightshades
- Simple sugars
- Consume:
- Oils rich in polyunsaturated fats (hemp seed, borage, etc.)
- Apple cider vinegar
- Coconut oil
But is it really this straightforward? If so, why do so many people still struggle with seborrheic dermatitis despite following this advice?
Exploring Specific Diets: Do They Hold the Key?
Beyond general advice, numerous specific diets are touted as quick fixes for seborrheic dermatitis. These diets often appear in online research and forums:
- Ketogenic diet
- Low carbohydrate diet
- Specific carbohydrate diet
- Lectin avoidance diet
- Anti-candida diet
The problem? These diets often contradict each other, making a universal “cure-all” diet unlikely.
Instead of chasing a single, elusive answer, a more effective approach is to evaluate each dietary option, understand its underlying principles, and then decide if it’s worth considering for your individual needs.
Previous Insights on Diet and Seborrheic Dermatitis
A previous article highlighted individual cases where dietary changes reduced seborrheic dermatitis symptoms. However, relying solely on individual stories can be misleading and add to the confusion. This article aims for a more evidence-based, systematic approach.
What Does the Medical Research Say About Diet and Seborrheic Dermatitis?
Moving past anecdotal evidence, let’s examine what medical literature reveals about the connection between diet and seborrheic dermatitis. While research in this area is limited, several key studies offer valuable insights.
Early research, though primarily theoretical, explored potential links and considerations. More recent questionnaire-based studies have attempted to identify dietary patterns associated with seborrheic dermatitis, with varying degrees of success.
Here’s a brief overview of four relevant studies:
Blood Levels of Vitamin E, Polyunsaturated Fatty Acids of Phospholipids, Lipoperoxides and Glutathione Peroxidase in Patients Affected with Seborrheic Dermatitis [1]
- Published: 1991 (Italy)
- Participants: 90 individuals (30 healthy, 30 HIV+ with seborrheic dermatitis, 30 HIV- with seborrheic dermatitis)
- Focus: Analysis of fatty acids, vitamin E (antioxidant), lipoperoxides (oxidized fatty acids), and erythrocyte glutathione peroxidase (antioxidant) in blood.
- Key Findings (Seborrheic Dermatitis Groups):
- Decreased Antioxidants: Lower levels of Vitamin E and erythrocyte glutathione peroxidase.
- Decreased PUFA: Reduced dihomo-γ-linolenic acid, arachidonic acid, and docosahexaneoic acid.
- Increased Saturated and Monounsaturated Fatty Acids: Higher palmitic acid, stearic acid, and oleic acid.
- No difference in lipoperoxides.
- Researchers’ Conclusion:
- Seborrheic dermatitis is associated with abnormalities in PUFA synthesis, likely not diet-related but due to desaturase enzyme issues.
- Reduced antioxidants may be linked to lower PUFA or other factors like pancreatic enzyme output, selenium deficiency, or breakdown/excretion.
- Replacement of PUFAs with saturated fatty acids in the epidermis could be a key factor in seborrheic dermatitis symptoms.
Possible Nutrient Mediators in Psoriasis and Seborrheic Dermatitis [2, 3]
- Published: 1988 (Israel) – Two-part paper
- Part 1: General overview of psoriasis and seborrheic dermatitis, including existing treatments.
- Part 2: Focus on potential nutrient involvement in the progression of both conditions.
- Key Observations:
- EFA Deficiency Similarity: Striking similarities between essential fatty acid (EFA) deficiencies and both skin conditions.
- EFA Supplementation Ineffectiveness: EFA supplements haven’t shown strong results, suggesting either the deficiency isn’t significant enough or other related factors are more critical.
- Vitamin A and Beta-Carotene: Psoriasis patients don’t appear deficient in Vitamin A, but have reduced beta-carotene in blood and skin.
- Other Vitamins: Vitamins E, D, B1, and C could potentially play a role, but evidence is lacking.
- Biotin (B6): Biotin deficiency is linked to infantile seborrheic dermatitis, but its role in adults is unproven. B6 and B2 are important for PUFA desaturation, but deficiencies in seborrheic dermatitis or psoriasis haven’t been shown.
- Iron and Zinc: Impact PGE concentrations and could be involved, but specific evidence is needed.
- Overall Conclusion: The paper highlights areas for further research but doesn’t provide definitive conclusions about specific nutrients and their role.
Association between Diet and Seborrheic Dermatitis: A Cross-Sectional Study [4]
- Published: 2018 (Netherlands)
- Data Source: Rotterdam Study (long-term study since 1990)
- Participants: 4,379 (636 with seborrheic dermatitis) – Middle-aged and elderly (average age 68.9 years)
- Dietary Patterns: Categorized into Western, fruit-rich, vegetable-rich, and high-fat diets.
- Key Findings:
- No Antioxidant-Seborrheic Dermatitis Link: No relationship found between dietary antioxidants and seborrheic dermatitis, contrary to expectations.
- Western Diet in Women: Higher seborrheic dermatitis incidence in women consuming a Western diet.
- Fruit-Rich Diet: Lower seborrheic dermatitis incidence with diets rich in fresh fruit.
- Vegetable and High-Fat Diets: No significant relationship found.
Relationship Between Diet and Seborrheic Dermatitis [5]
- Published: 2018 (Turkey)
- Participants: 101 (51 with seborrheic dermatitis)
- Dietary Intake Categories: 21 categories (meat, processed meat, chicken, fish, etc.)
- Surprising Finding: Vegetable intake associated with higher rates of seborrheic dermatitis.
- Directionality Issue: Study participants already had seborrheic dermatitis, making it hard to determine if diet caused the condition or if people changed their diet because of the condition (e.g., eating more vegetables to be healthier).

My Personal Experience: Diet and Seborrheic Dermatitis Control
Like many others struggling with seborrheic dermatitis, I explored numerous diets, driven by the desperation to find relief. The impact of this condition on daily life can be significant, pushing individuals to try almost anything. My journey through various dietary approaches was extensive and often frustrating.
The only diet that consistently improved my seborrheic dermatitis was extremely restrictive: a diet of only raw carrots and apples (or fasting). Within a day, my skin would stabilize, and inflammation would decrease. However, this unsustainable approach highlighted a key point: diet could influence my seborrheic dermatitis.
While other, more balanced diets recommended online had no noticeable effect for me, the temporary success with the carrot and apple diet fueled my belief in dietary intervention. Even with years of managing my skin through lifestyle adjustments and topical treatments, the idea of achieving lasting relief from seborrheic dermatitis through a deeper understanding of diet remains compelling.
Developing a Systematic Dietary Approach for Seborrheic Dermatitis
Given the limited definitive research and the theoretical nature of the diet-seborrheic dermatitis connection, a structured, self-analytical approach is likely the most beneficial.
Based on the research reviewed, three primary components appear most relevant (in order of potential importance):
- Essential Fatty Acid (EFA) Availability and Synthesis
- Lipid Oxidation and Antioxidant Availability
- Mineral and Vitamin Balance
Let’s examine each of these factors in detail and explore how to assess and potentially address them to manage your seborrheic dermatitis.
1. Essential Fatty Acids: Fueling Healthy Skin from Within
Essential fatty acids (EFAs) and their role in inflammation and skin health have been discussed in detail in previous articles:
Key Takeaways on Essential Fatty Acids:
- Dietary Necessity: EFAs are fats our bodies can’t produce and must obtain from food. True deficiency is rare in developed countries, but imbalances are common.
- Omega-3 to Omega-6 Imbalance: Modern Western diets often have a skewed ratio of omega-6 to omega-3 fatty acids, contributing to chronic inflammation [6, 7].
- Internal Synthesis: Our bodies convert dietary EFAs into other fatty acids needed for various functions via enzyme-driven processes [8, 9, 10]. Disruptions in these processes are linked to skin disorders [11].
While direct evidence linking EFAs to seborrheic dermatitis is limited, the condition’s close relationship with sebum production [] and EFAs’ influence on sebum quality and output [] suggests a strong potential connection. Furthermore, diet is a readily modifiable factor, making EFA balance a worthwhile area to explore.
Actionable Steps: Improving Omega-3 to Omega-6 Ratio
The primary goal is to correct the omega-6 to omega-3 imbalance prevalent in many diets.
Simple Strategies:
- Limit Vegetable Oils: Reduce or eliminate common vegetable oils high in omega-6s (soybean, corn, sunflower, etc.).
- Increase Fatty Fish Intake: Consume fresh fatty fish (salmon, mackerel, sardines) more frequently.
Improvements may not be immediate [12], but over time, rebalancing your omega intake can reduce overall inflammation, potentially benefiting seborrheic dermatitis.
For more detailed guidance on improving your omega-3 to omega-6 ratio, refer to these resources:
Actionable Steps: Enhancing Essential Fatty Acid Synthesis
Optimizing your body’s ability to process dietary fats and synthesize specific fatty acids is crucial for overall health and skin function. This metabolic process directly impacts sebum production [].
While the exact lipids and fatty acids most relevant to seborrheic dermatitis are still under investigation, general dietary and lifestyle recommendations can support healthy lipid metabolism:
- Increase Vitamin A, Fiber, and Polyphenol Intake: [13, 14, 15] Focus on colorful fruits and vegetables.
- Eliminate Processed Foods: [16] These often contain unhealthy fats and additives that can disrupt metabolic processes.
- Manage Stress: [17] Chronic stress can negatively impact various bodily functions, including metabolism.
- Balance Omega-3 to Omega-6 Ratio: [18] As discussed above.
- Increase Physical Activity: [19] Exercise supports overall metabolic health.
- Evaluate Thyroid Function: [20, 21] Thyroid hormones play a role in metabolism.
- Reduce Alcohol Consumption: [22, 23] Alcohol can interfere with metabolic processes.
For more in-depth information on supporting fatty acid synthesis, see: .
2. Antioxidant Availability: Combating Oxidative Stress
Regarding antioxidants, a diet rich in fruits and vegetables is generally considered sufficient to meet antioxidant needs [].
While supplements are an option, moderation is key. Free radicals play a role in immune function, and excessive antioxidant intake can interfere with these processes [24, 25]. Fat-soluble antioxidants like Vitamin E and Vitamin A can even become toxic in high doses [26, 27].
A balanced approach is best: focus on a diet rich in antioxidant-rich foods and consider low-risk antioxidant supplements:
- Vitamin C
- Grape seed extract
- Turmeric
This list is intentionally concise to avoid overwhelming complexity. Share your thoughts on other beneficial antioxidants in the [comments section][1].
Actionable Steps: Reducing External Free Radical Sources
Alongside increasing antioxidant intake, minimizing exposure to sources of oxidized fats and high-glycemic index foods is crucial. These factors contribute to unnecessary oxidation within the body.
Limit or Avoid:
- Fried and deep-fried foods
- Packaged/processed foods
- Old nuts and seeds (check dates for freshness)
- Refined vegetable oils (often lacking natural vitamin E)
- Sugar, soda, and sugary treats
By combining increased antioxidant intake from whole foods with reducing exposure to oxidative stressors, you can support your body’s natural defense against free radicals.
3. Mineral and Vitamin Availability: Addressing Potential Deficiencies
Self-supplementing with vitamins and minerals without medical guidance is generally not recommended due to potential risks of toxicity and imbalances.
If you suspect specific deficiencies, consult your doctor and request appropriate testing before starting any supplements.
Focusing on whole food sources, evidence suggests that increasing intake of the following foods may be beneficial for mineral and vitamin intake relevant to skin health:
- Fresh Fatty Fish: Selenium, Vitamin D, Vitamin E
- Carrots, Sweet Potatoes, Dark Leafy Greens: Vitamin A
- Quality Fresh Nuts and Seeds (in moderation): Vitamin E, Selenium
- Bone Broth: Assortment of minerals [28]
These are general recommendations. Review your current diet and identify areas where you can incorporate more nutrient-rich whole foods.
4. Considering Short-Chain Fatty Acids: Gut Health and Immunity
Emerging research highlights the importance of gut health and short-chain fatty acids (SCFAs) in overall health, including potentially skin health.
What are Short-Chain Fatty Acids?
SCFAs are fatty acids with fewer than six carbon atoms. While some foods contain small amounts, the majority are produced in the colon through microbial fermentation of dietary fiber [29].
SCFAs play critical roles in:
My hypothesis is that SCFAs may influence seborrheic dermatitis by modulating the immune response, particularly T cells, and reducing hyperactivity [33].
Disruptions in gut microflora, potentially from diet, stress, infections, or medications, could lead to reduced SCFA production and increased inflammatory compounds. This imbalance might contribute to an inflammatory immune response relevant to seborrheic dermatitis.
Actionable Steps: Increasing Short-Chain Fatty Acid Availability
To potentially increase SCFA production and improve gut health:
- Increase Dietary Fiber: Focus on fiber-rich foods, especially types known to promote beneficial gut bacteria.
While direct evidence linking SCFAs deficiency to seborrheic dermatitis is lacking, recent studies suggest SCFAs’ role in skin immunity:
- Sodium Butyrate: Regulates skin immune response and reduces sensitivity to antigens [34].
- Sodium Butyrate and Lactic Acid Bacteria: Alleviated atopic dermatitis symptoms in mice [35].
Even without direct proof of skin-level SCFA impact from dietary changes, improving gut health through fiber intake has numerous overall health benefits.

Addressing Suspected Food Allergies/Sensitivities
Food allergies, sensitivities, and intolerances are often discussed in relation to seborrheic dermatitis. While evidence is primarily anecdotal, this area may be relevant for some individuals, especially if you’ve noticed a connection between specific foods and skin symptoms.
However, relying solely on anecdotal advice and jumping to conclusions can be detrimental.
The Pitfalls of Self-Diagnosis:
Imagine this scenario:
- You read a compelling story about someone clearing their seborrheic dermatitis by avoiding gluten.
- You decide gluten is your trigger and adopt a gluten-free diet.
- Initially, your skin improves, reinforcing your belief in gluten sensitivity.
- But after a week, your symptoms return despite strict gluten avoidance.
- You attribute flare-ups to accidental gluten exposure, intensifying your efforts.
- Your skin remains unpredictable, and you question if gluten is truly the culprit.
- You reintroduce gluten, still anxious and unsure.
The result? Persistent skin issues and added food anxiety.
Research even suggests that self-perceived food intolerances can become as problematic as actual allergies, triggering immune responses through psychological mechanisms [36, 37, 38].
A More разумный Approach:
- Medical Testing: Consult your doctor, discuss your concerns, and request appropriate allergy/sensitivity testing.
- Food Journal: Keep a detailed record of your food intake and daily symptom severity for 4-6 weeks.
Combining medical testing with a food journal provides objective data to guide your dietary decisions and reduce unnecessary anxiety.
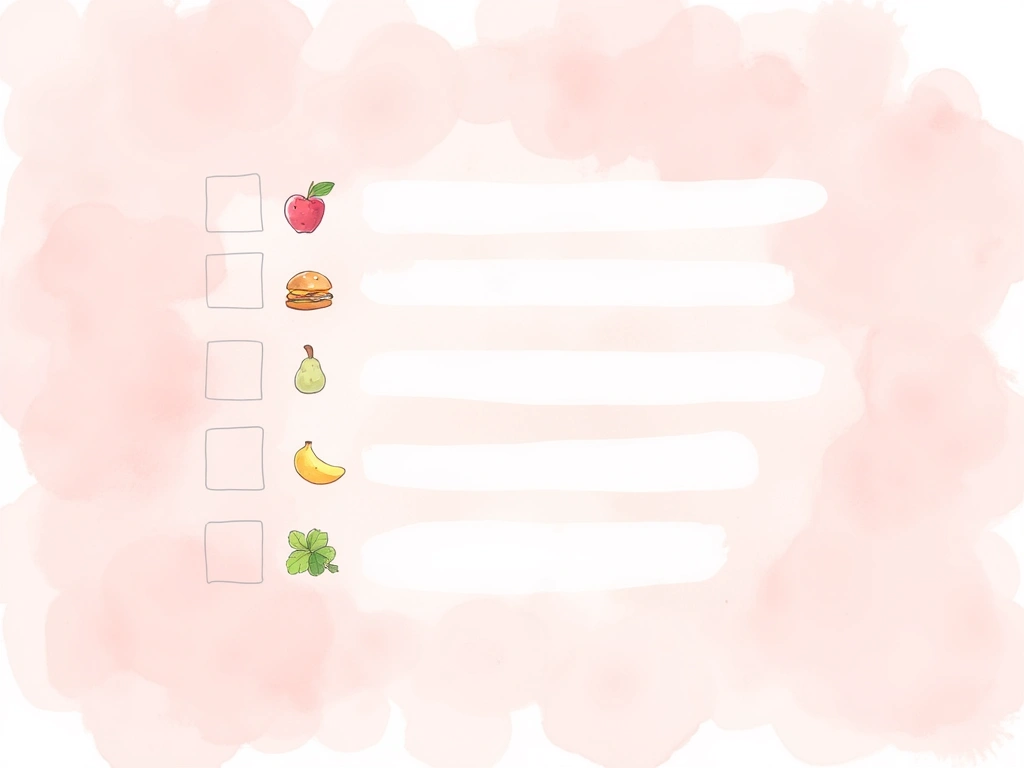
Implementing Your Seborrheic Dermatitis Dietary Strategy: An Action Plan
This section translates the research and insights into a practical plan you can implement to potentially manage your seborrheic dermatitis through diet.
Dietary Objectives:
- Fatty Fish: Aim for at least two meals per week featuring fresh fatty fish as the main protein source. Excellent source of anti-inflammatory omega-3 fatty acids.
- Refined Carbohydrates: Drastically reduce or eliminate refined carbohydrates (white bread, sugary drinks, processed snacks). Helps regulate insulin levels and potentially sebum output.
- Added Vegetable Oils: Minimize or eliminate added vegetable oils high in omega-6s (soybean, corn, sunflower). Flaxseed oil can be used in moderation, but fresh flaxseeds are preferable. Reduces excess omega-6 intake.
- Lactose-Rich Products: Reduce consumption of milk and other high-lactose dairy. Butter and cream, with lower lactose content, may be less problematic. Overlaps with refined carbohydrate reduction and may have similar benefits.
- Beta-Carotene Rich Foods: Consume 3-4 servings daily of foods rich in beta-carotene (carrots, sweet potatoes, leafy greens) for the first 3-4 weeks, then reduce to 2-3 servings. Supports lipid metabolism.
- Fiber-Rich Vegetables: Include 3-4 servings daily of fiber-rich vegetables. Fiber from grains may be less effective. Promotes gut health and SCFA production.
Supplementary Lifestyle Objectives:
- Activity Tracker: Use an activity tracker to ensure consistent movement throughout the day. Supports hormone balance, metabolism, and insulin sensitivity.
- Stress Management: Develop stress-coping strategies. Focus on transforming stress into positive energy rather than avoidance. Stabilizes immune function and reduces systemic inflammation.
- Re-evaluate Anecdotal Reports: Be critical of online testimonials and anecdotal advice. Misinformation can increase anxiety and misguide your approach.
- Sun Exposure (Moderate): Obtain safe sun exposure. Supports Vitamin D production (hormone regulation) and circadian rhythm.
For Suspected Food Sensitivities:
- Food Journaling: Maintain a detailed food journal for 4-6 weeks to identify potential symptom correlations. Essential for uncovering individual food triggers.
- Medical Testing: Consult your healthcare provider for appropriate medical testing. Eliminates guesswork and provides objective data.
Personalize Your Action Plan
Remember, this is a flexible framework. Adjust the plan to fit your individual needs and preferences.
For further reading on related topics, explore these resources:
If you have any questions as you implement this plan, please ask in the [comments section below][1].
Section Update in Progress
This section will be expanded with practical resources like worksheets detailing omega-3 rich fish, beta-carotene sources, stress reduction techniques, and more.

Summary: Key Takeaways for Seborrheic Dermatitis Diet
This article explored the potential role of diet in managing seborrheic dermatitis, prioritizing evidence-based information over anecdotal claims.
Key Points:
- Anecdotal Diet Cures: Online reports of dietary cures for seborrheic dermatitis are common but often lack scientific backing.
- Common Dietary Suggestions: Frequently recommended changes include avoiding dairy, gluten, nightshades, and sugar, while increasing healthy oils and apple cider vinegar.
- Limited Medical Literature: Research on diet and seborrheic dermatitis is limited and often theoretical.
- Key Dietary Factors: Dietary lipids, antioxidants, and vitamins/minerals influencing lipid metabolism are likely most impactful.
- Omega-3 to Omega-6 Balance: Prioritize rebalancing omega-3 and omega-6 fatty acid intake.
- Support Lipid Metabolism: Vitamin A, fiber, polyphenols, a clean diet, stress management, exercise, thyroid health, and moderate alcohol intake support healthy lipid utilization.
- Antioxidant-Rich Diet: A diet rich in fruits and vegetables provides sufficient antioxidants to combat oxidative stress.
- Short-Chain Fatty Acids and Gut Health: Specific dietary fiber can promote beneficial gut bacteria, increasing SCFA production, stabilizing immunity, and reducing inflammation.
- Address Food Sensitivities Systematically: Use food journaling and medical testing to identify potential food triggers rather than relying on self-diagnosis.
Thank you for exploring the potential of diet in managing seborrheic dermatitis. I hope this information is relevant and helpful for you. Share your thoughts, ideas, and questions in the comments section below.
Have you experimented with/what are you thoughts on FMT to re-balance the microflora?
Reply PermalinkHey there people! how’s going? any new stories to share in 2020? hope to hear soon from you, have a nice day!
Reply Permalink