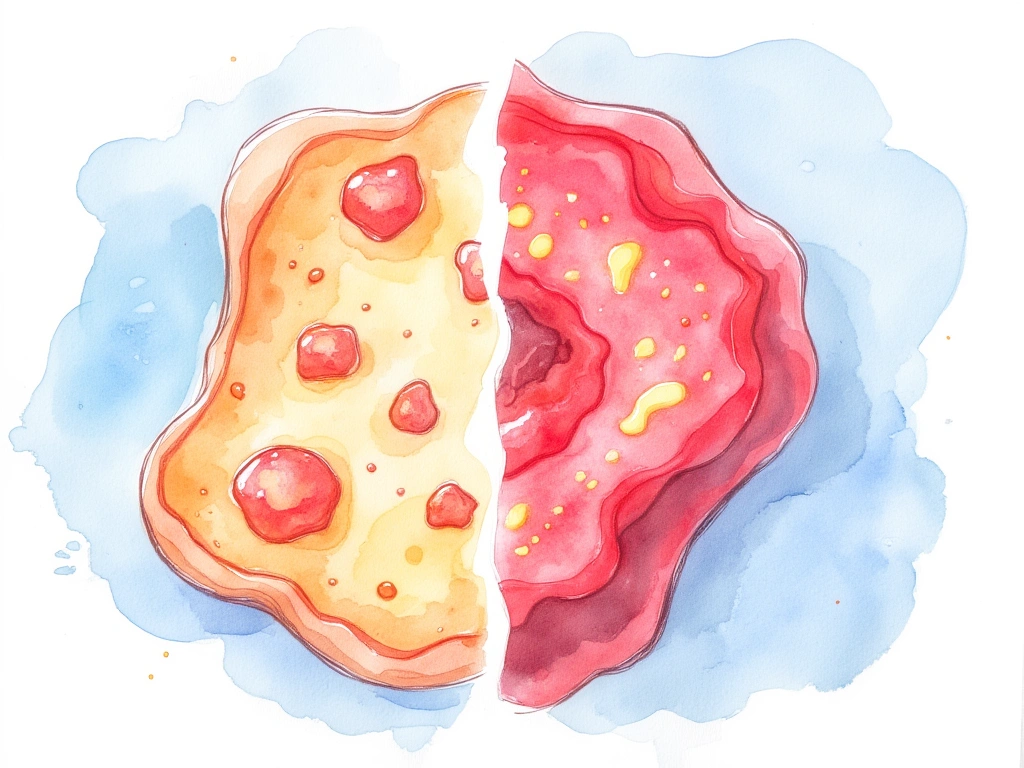
- Redness and irritation? Seborrheic dermatitis and rosacea can look similar, but they’re different skin conditions.
- Oily vs. Dry? Seborrheic dermatitis is often greasy, while rosacea tends to be dry.
- Flakes vs. Bumps? Seborrheic dermatitis features flaky scales, rosacea presents acne-like bumps.
- Itchy vs. Stinging? Seborrheic dermatitis is typically itchy, rosacea often stings or burns.
- Scalp vs. Cheeks? Seborrheic dermatitis favors scalp and hairline, rosacea targets cheeks and nose.
Seborrheic dermatitis and rosacea are common inflammatory skin conditions that can be easily confused. Both can cause facial redness, irritation, and flaking, leading to uncertainty about which condition you might be experiencing. However, understanding their distinct underlying causes, symptoms, and treatments is crucial for effective management.
This guide provides a detailed, side-by-side comparison to help you distinguish between seborrheic dermatitis and rosacea, ensuring you can seek the right approach for clearer, healthier skin.
Quick Takeaway: Seborrheic dermatitis and rosacea both cause facial redness but differ significantly in oiliness, scaling, breakouts, location, itchiness, and eye involvement. Accurate diagnosis based on these differences is key for effective treatment, whether antifungal for seborrheic dermatitis or antibiotic for rosacea. Misdiagnosis can lead to ineffective treatment and ongoing social and emotional impacts, highlighting the importance of precise clinical distinction.

Understanding Seborrheic Dermatitis
Seborrheic dermatitis is a chronic inflammatory skin condition characterized by red, flaky, and greasy patches, particularly in areas rich in oil glands. Common areas affected include the scalp, face, upper chest, and back. It’s estimated that up to 5% of adults may experience seborrheic dermatitis [1].
Common Symptoms:
- Red, inflamed, scaly, and flaky skin
- Greasy skin with yellowish or whitish scales or crusts
- Itching
- Cracking and fissures in the skin
Seborrheic dermatitis often makes its first appearance as cradle cap (dandruff) in infancy. While it often improves by adulthood, it can still flare up periodically, especially during stressful times. In adults, it is observed more frequently in men than in women [2].
What Causes Seborrheic Dermatitis?
The exact cause of seborrheic dermatitis remains unclear. However, the yeast Malassezia, a fungus that naturally resides on the skin, is believed to play a significant role. Overgrowth of this yeast in oily areas is thought to trigger inflammation and the characteristic symptoms of seborrheic dermatitis [3].

Understanding Rosacea
Rosacea is another chronic skin condition, estimated to affect more than 16 million Americans [4]. It primarily affects the central face, causing redness, swelling, and acne-like breakouts. Many individuals with rosacea also report stinging, burning sensations, and increased skin sensitivity.
Rosacea Subtypes:
Rosacea is classified into four subtypes:
- Erythematotelangiectatic Rosacea: Characterized by persistent redness and visible blood vessels.
- Papulopustular Rosacea: Features redness accompanied by acne-like breakouts.
- Phymatous Rosacea: Leads to thickened skin and irregular surface texture.
- Ocular Rosacea: Involves eye irritation, dryness, and redness.
Rosacea typically emerges between the ages of 30 and 60 and is more prevalent in women [5]. However, men often experience more severe symptoms [6].
What Causes Rosacea?
The exact cause of rosacea is not fully understood. Several factors are believed to contribute, including vascular changes, immune system dysfunction, skin barrier abnormalities, and the potential role of microscopic skin mites [7].
Side-by-Side Comparison: Seborrheic Dermatitis vs. Rosacea
While seborrheic dermatitis and rosacea share some overlapping symptoms, key differences can help distinguish between them. Here’s a comparative overview:
| Comparison Dimension | Seborrheic Dermatitis | Rosacea |
|---|---|---|
| Prevalence | 1-5% of adults | Up to 10% of adults |
| Age of Onset | Infancy or adulthood | 30-60 years |
| Sex Predominance | Males > Females | Females > Males |
| Areas Affected | Scalp, face, chest, back | Central face (cheeks, nose, chin, forehead) |
| Appearance | Red, greasy, flaky, scaly | Red, swollen, acne-like breakouts |
| Itchiness | Usually itchy | Sometimes itchy, more stinging/burning |
| Cause | Fungal overgrowth (Malassezia) | Unclear – vascular, immune, mites potentially involved |

Key Symptom Differences
Despite some similarities like facial redness and irritation, distinct symptom variations are crucial in differentiating seborrheic dermatitis from rosacea.
1. Greasiness and Scaling
A hallmark of seborrheic dermatitis is greasy skin accompanied by yellowish scales and flakes. The skin often has a shiny appearance due to excess oil. In contrast, rosacea typically does not involve excessive oiliness. Instead, the skin may feel dry and tight.
2. Acne-Like Breakouts
Small red bumps and pimples are not typical in seborrheic dermatitis but are a common feature of rosacea, particularly in papulopustular rosacea. This difference is a significant distinguishing factor.
3. Distribution of Redness
The location of redness differs between the two conditions. Rosacea redness is most prominent on the central face – cheeks, nose, chin, and central forehead. Seborrheic dermatitis tends to spare these areas, favoring the hairline, eyebrows, ears, and skin around the nose and mouth.
4. Itchiness vs. Stinging
Seborrheic dermatitis is often characterized by significant itchiness, especially on the scalp. Rosacea, while it can sometimes itch, is more commonly associated with stinging, burning, and tenderness.
5. Eye Involvement
Ocular rosacea can cause eye symptoms like dryness and irritation. Seborrheic dermatitis does not directly affect the eyes, making eye involvement a key differentiator.
Symptom Summary Table
| Key Differences in Symptoms | Seborrheic Dermatitis | Rosacea |
|---|---|---|
| Greasiness and Scaling | Greasy skin with yellowish scales and flakes | Lack of excessive oiliness, may feel dry and tight |
| Acne-Like Breakouts | Not characteristic | Small red bumps and pimples common |
| Distribution of Redness | Favors hairline, eyebrows, ears, skin bordering nose/mouth | Most prominent on cheeks, nose, chin, central forehead |
| Itchiness | Often itchy, especially on the scalp | Stinging and tenderness, itchiness less common |
| Eye Involvement | Does not directly affect the eyes | Can cause dryness, irritation in the eyes |

Distinguishing Between Seborrheic Dermatitis and Rosacea: A Closer Look
Accurately identifying whether you have seborrheic dermatitis or rosacea is essential for effective treatment. Consider these points when evaluating your symptoms:
- Symptom Type: Is your skin greasy with yellowish flakes (Seborrheic Dermatitis) or dry and tight, possibly with bumps (Rosacea)? Note the specific characteristics of your skin.
-
Redness Pattern: Where is the redness most prominent? Hairline, eyebrows, and around the mouth suggest seborrheic dermatitis. Cheeks, nose, and central forehead point towards rosacea.
-
Breakouts: Are acne-like bumps present? Their presence is more indicative of rosacea.
-
Sensations: Is itching the primary discomfort, or do you experience stinging and burning? Itchiness is more common in seborrheic dermatitis, while stinging and burning are typical of rosacea.
-
Eye Symptoms: Are your eyes dry or irritated? This could suggest ocular rosacea.
-
Age and Gender: Consider your age and gender. While not definitive, rosacea is more common in women aged 30-60, and seborrheic dermatitis is slightly more common in men and can start in infancy.
For a definitive diagnosis, consult a dermatologist. Self-diagnosis can be inaccurate, and professional evaluation ensures you receive the correct treatment plan.
Treatment Strategies
Diagnosis of both seborrheic dermatitis and rosacea is primarily based on a doctor’s evaluation of your clinical history and a physical examination. Specific lab tests are not typically required, though skin biopsies may occasionally be performed to rule out other conditions.
Effective management hinges on tailoring treatments to the specific condition:
Seborrheic Dermatitis Treatment: While there’s no cure for seborrheic dermatitis, it can be effectively managed. Treatments focus on controlling fungal overgrowth using antifungal creams, shampoos, and sometimes oral medications. Gentle skincare practices, stress management, and avoiding triggers are also important for long-term control [8].
Rosacea Treatment: Rosacea also lacks a definitive cure, but treatments aim to minimize flare-ups and manage symptoms. Options include oral and topical antibiotics, azelaic acid, and isotretinoin. Laser therapy can be beneficial for reducing redness and flushing in some individuals [6]. Lifestyle adjustments are also crucial in managing rosacea.
Misdiagnosis can lead to ineffective treatments and persistent symptoms. Therefore, accurately distinguishing between seborrheic dermatitis and rosacea is vital for successful management.
Diagnosis and Treatment Summary Table
| Diagnosis and Treatment | Seborrheic Dermatitis | Rosacea |
|---|---|---|
| Diagnostic Approach | Clinical history and examination findings | Clinical history and examination findings |
| Laboratory Tests | No definitive laboratory tests | No definitive laboratory tests |
| Skin Biopsies | Occasionally to rule out other conditions | Occasionally to rule out other conditions |
| Management Approach | Incurable but controllable | No cure, aims to minimize outbreaks |
| Primary Treatments | Antifungal creams, shampoos, oral medication | Oral and topical antibiotics, azelaic acid, isotretinoin |
| Additional Treatments | Gentle skin care, stress management, trigger avoidance | Laser therapy, lifestyle modifications |
The Broader Impact of Skin Conditions
Skin disorders like seborrheic dermatitis and rosacea can have impacts that extend beyond the skin itself, significantly affecting quality of life. Social anxiety, embarrassment, depression, and work-related stress are frequently reported secondary consequences [9].
Accurate diagnosis is the first step toward not only medical treatment but also providing necessary psychological support. This holistic approach can help individuals develop effective coping strategies for living with chronic skin conditions. Patient education and support groups also offer valuable peer support and resources.
Conclusion: Precision is Key for Effective Management
In conclusion, while seborrheic dermatitis and rosacea share symptoms like facial redness and irritation, they are distinct conditions requiring different management approaches. Careful attention to subtle symptom differences and a thorough clinical history are crucial for accurate diagnosis. Misdiagnosis can result in ineffective treatments and prolonged discomfort, emphasizing the importance of clinical precision.
Ongoing dermatological research promises to deepen our understanding of the molecular mechanisms driving these conditions, potentially leading to more targeted and effective therapies in the future.
The impact of skin disorders is not limited to physical symptoms; it significantly affects emotional well-being. Addressing these emotional aspects through patient education, support systems, and comprehensive disease management is essential. Recognizing these conditions as more than just cosmetic concerns, but as potential contributors to social anxiety, embarrassment, and depression, underscores the need for holistic and compassionate care. As diagnostic tools and treatments advance, integrating research, patient experiences, and innovative therapies will be crucial in improving the lives of those affected by seborrheic dermatitis and rosacea.
“`
No Comments
Be the first to start a conversation