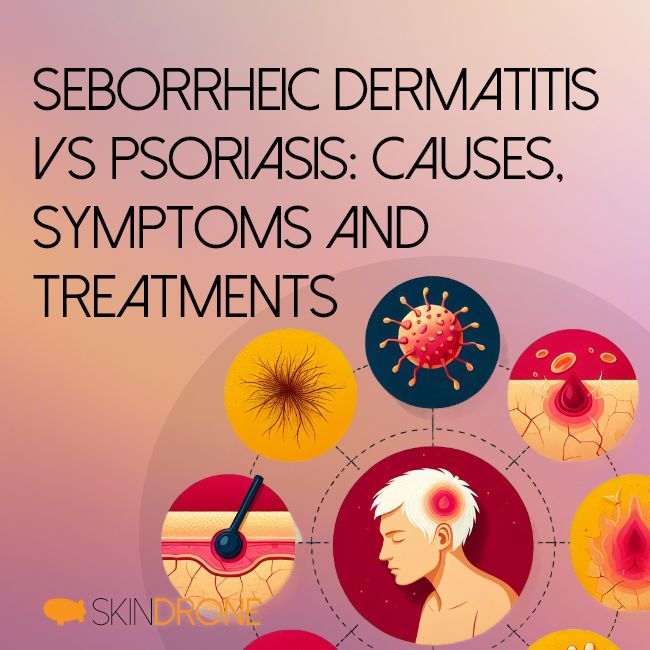
This article will provide an in-depth examination of seborrheic dermatitis and psoriasis to highlight their key characteristics. It will outline the methods used by doctors to tell them apart and summarize the implications of misdiagnosis. The article concludes with practical lifestyle measures patients can take to alleviate symptoms alongside medical treatment.
In-Depth Look at Seborrheic Dermatitis
Seborrheic dermatitis is a chronic skin condition marked by flaking, scaling, and erythema (redness) [2]. It most often affects sebum-rich areas including the scalp, central face, and upper back.
Symptoms and Progression
The most common symptoms are [3]:
- Red, greasy skin covered with flaky white or yellow scales
- Patches of dry, irritated skin
- Itchiness and burning sensation
Onset is typically gradual. Symptoms may fluctuate in severity and worsen with stress or changes in hormone levels [4]. Without treatment, symptoms persist long-term with periodic flares.
Infants within the first 3-4 months of life commonly get cradle cap. This form clears spontaneously after about a year [4]. Seborrheic dermatitis then reappears during puberty, persisting through adulthood with peak severity after age 50 [4].
Treatment Approach
First-line treatments are topical antifungal agents containing ketoconazole, zinc pyrithione, selenium sulfide, or salicylic acid [5]. These help curb colonization of Malassezia yeasts implicated in seborrheic dermatitis [6].
For more resistant cases, topical corticosteroids and calcineurin inhibitors may be prescribed alongside antifungals. Phototherapy is another option. Dietary modifications to exclude food triggers can help reduce flare-ups.
With appropriate treatment, seborrheic dermatitis can be controlled though difficult to completely cure [1]. Periodic returns of symptoms are common, especially with fluctuations in immune status, stress levels, or hormonal changes [3].
In-Depth Look at Psoriasis
Psoriasis is an autoimmune condition causing rapid buildup of skin cells. This results in inflamed, scaly plaques on the skin’s surface [7].
Symptoms and Progression
The most characteristic signs are [8]:
- Patches of red, scaly, inflamed skin
- Silvery-white scales or plaque buildup on affected areas
- Pitting, splitting, or loosening of fingernails and toenails
- Joint pain, stiffness, and swelling (psoriatic arthritis)
In most cases, psoriasis follows a relapsing-remitting course with disease flares interspersed by periods of remission. Once diagnosed, psoriasis is generally lifelong though individual prognosis varies [9].
Types of Psoriasis
There are several variants of psoriasis to distinguish:
Plaque psoriasis – The most common form (90% of cases) marked by raised, inflamed lesions covered with silvery-white scales typically occurring on the knees, elbows, scalp, and torso [10].
Guttate psoriasis – Small, drop-shaped sores appear on the trunk, arms, legs, and scalp. Often follows a bacterial throat infection. Tends to resolve spontaneously after several weeks [11].
Inverse/flexural psoriasis – Smooth, red lesions form in skin folds around genitals, armpits, and under the breasts or buttocks. Lack the thick scale seen in plaque psoriasis due to moisture, friction, and absence of air.
Pustular psoriasis – White, pus-filled blisters surrounded by red skin. Tends to have cyclical flares. Can be life-threatening if widespread due to loss of skin barrier. Requires urgent treatment [12].
Erythrodermic psoriasis – Severe, widespread inflammation and exfoliation of most of the skin’s surface. Can develop suddenly in plaque psoriasis or from withdrawal of corticosteroid treatment. Causes life-threatening protein and fluid loss.
Treatment Approach
Topical agents remain first-line therapy for mild to moderate psoriasis:
- Corticosteroids – Powerful anti-inflammatory effect but risks skin damage with long-term use [13].
- Vitamin D analogs – Help normalize excessive growth of skin cells [14].
- Tazarotene – Synthetic retinoid that reduces inflammation.
- Anthralin – Suppresses skin cell turnover [15].
- Moisturizers – Soothe and hydrate irritated skin.
For moderate to severe cases, phototherapy with controlled doses of UV light helps dampen skin cell overproduction and inflammation [16].
Oral or injectable systemic medications like methotrexate, cyclosporine, and biologic agents directly target pathological inflammatory pathways in psoriasis. However, these treatments require careful monitoring for cumulative organ toxicity and side effects [9].

Direct Comparison: Seborrheic Dermatitis vs Psoriasis
Despite some visual resemblance, seborrheic dermatitis and psoriasis differ in their underlying mechanisms, distribution patterns, and triggers.
| Seborrheic Dermatitis | Psoriasis | |
|---|---|---|
| Pathogenesis | Exaggerated skin reaction to commensal yeast (Malassezia spp.) [6] | Autoimmune disorder causing epidermal hyperplasia and inflammation mediated by IL-17/IL-23 pathway [7] |
| Characteristics | Greasy, yellow scales with underlying redness | Thick silvery-white scales with well-demarcated borders |
| Locations | Central face, scalp, upper back, and chest. Spares distal limbs. | Variable. Commonly knees, elbows, trunk, and scalp. Can occur anywhere. Nail changes only in psoriasis. |
| Course | Fluctuating symptoms with periodic flares. | Chronic relapsing course. |
| Triggers | Changes in sebum production, humidity, skin pH alterations, stress, immunosuppression | Genetic predisposition with possible environmental triggers like infections, medication, skin trauma, stress, and cold weather [17, 18]. |
| Associated conditions | Higher rates of metabolic disease and depression [1] | Psoriatic arthritis (10-30% cases) [19]. Increased cardiovascular risks. High psychiatric comorbidity. |
| Treatment | Topical antifungals, topical steroids. Oral antifungals rarely needed. | Topical therapies, phototherapy, and systemic immunomodulators like methotrexate, cyclosporine, biologics depending on severity. |
| Prognosis | Persisting, difficult to cure. Controlled with maintenance treatment. | Lifelong condition with alternating remissions and flares. Prognosis variable. |

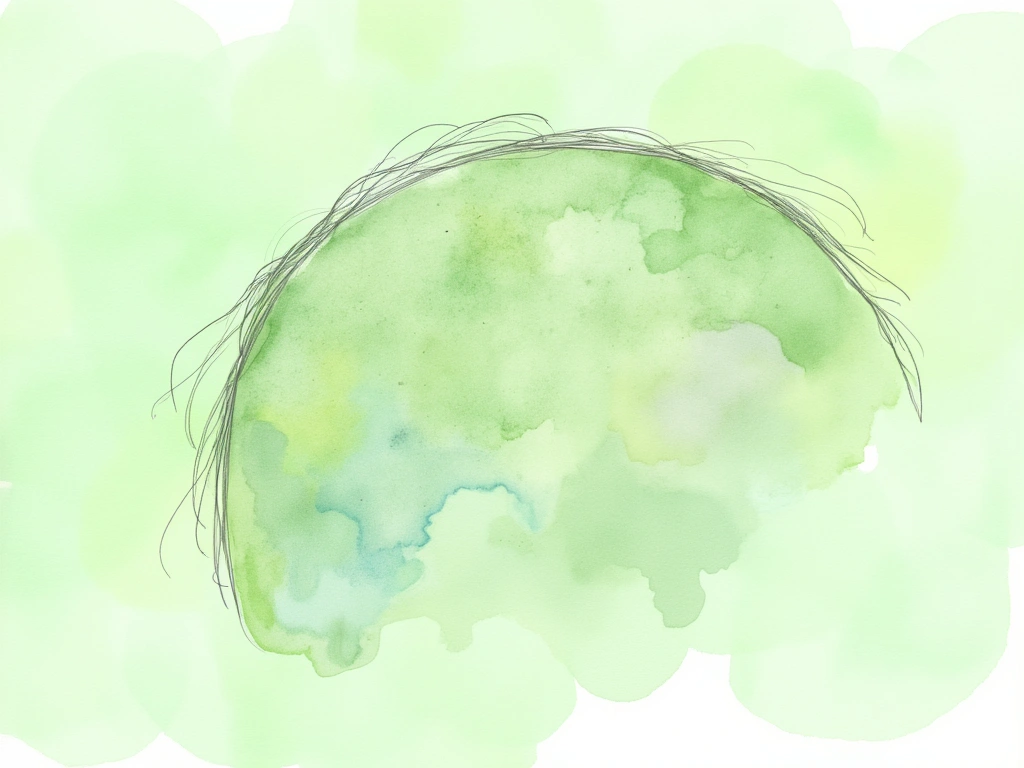
Scalp Involvement: Seborrheic Dermatitis vs Psoriasis
Seborrheic dermatitis presents as greasy yellow flakes with underlying redness. Hair damage is generally reversible.
Key features:
- Mild to moderate scaling
- Itchiness is common
- No permanent hair loss
- Treatment involves topical antifungals, intermittent topical steroids [2]
Scalp psoriasis causes thick, clearly demarcated silvery plaques that bleed easily. Risk of permanent hair loss is higher.
Key features:
- Dense, adherent scales
- Increased fragility and breakage of hair [10]
- Higher rates of hair loss
- Potential psoriatic arthritis [19]
- Phototherapy, vitamin D derivatives, and topical steroids more often needed [13]
Distinguishing features aid diagnosis of ambiguous cases:
| Seborrheic Dermatitis | Scalp Psoriasis |
|---|---|
| Milder inflammation [20] | Thick plaques [9] |
| Greasy yellow scales | Prominent silvery scales [10] |
| Central involvement on scalp | Any site on scalp [8] |
| Reversible hair changes | Higher rates of permanent hair loss [10] |
| Rarely itchy [2] | Frequent itch [9] |
| No joint complaints | May have psoriatic arthritis [19] |

Misdiagnosis and Its Risks
Distinguishing seborrheic dermatitis from plaque psoriasis or scalp psoriasis can be challenging. However, incorrect diagnosis impairs effective treatment.
Due to its greasy scales and facial involvement, seborrheic dermatitis is sometimes mistaken for scalp psoriasis. Meanwhile, psoriasis on the body may be misidentified as seborrheic dermatitis. This is especially true with inverse and flexural psoriasis in the absence of thick plaques.
Misdiagnosing seborrheic dermatitis as psoriasis often prompts prescription of inappropriate systemic therapies or UVR phototherapy with their attendant side effects [21]. These aggressive treatments offer little added benefit if skin inflammation is actually driven by yeast overgrowth instead of autoimmunity.
Conversely, wrongly dismissing psoriatic disease delays initiating treatment to target IL-17 mediated inflammation early on. Unchecked disease can lead to cumulative damage to skin and joints as well as adverse physical and psychosocial sequelae. Distinguishing other variants like pustular and erythrodermic psoriasis is also critical given their potential to cause life-threatening electrolyte abnormalities [12].
Careful history taking and physical examination aids diagnosis by eliciting differences between their common sites of involvement, triggers and associated illnesses. Tricky cases may need skin biopsy or trial of antifungal therapy to rule out seborrheic dermatitis masquerading as one of the scaly eruptions of psoriasis.

Living with Seborrheic Dermatitis and Psoriasis
Coping with chronic inflammatory skin disease poses physical and emotional challenges for patients. Lifestyle measures to reduce flare triggers and optimize disease control are important adjuncts to medical therapy.
Lifestyle Adaptations
The following lifestyle strategies may help reduce symptoms:
- Stress management – Try relaxation techniques, counseling, or support groups to mitigate anxiety and depression.
- Avoid skin irritants – Use gentle cleansers. Wear smooth fabrics, avoid wool and synthetic materials.
- Moisturize skin – Apply fragrance-free moisturizers after bathing. Ointments seal in moisture better than lotions.
- Control alcohol intake – Alcohol can promote inflammation and interacts with some systemic psoriasis medication.
- Quit smoking – Smoking increases the risk for both conditions and may initiate disease in genetically predisposed people.
- Address infections – Promptly treat strep infections to help prevent guttate flares. Avoid unnecessary antibiotics when possible.
- Improve diet quality – An anti-inflammatory diet rich in produce, fibers, and omega-3 fatty acids may help dampen symptoms.
- Optimize vitamin D – Low vitamin D worsens several autoimmune conditions. Use sun protection but ensure adequate daily intake through UV exposure, fortified foods, or supplementation.
- Consider supplements – Herbal remedies like aloe vera, milk thistle, or curcumin may provide relief for some people, but clinical evidence is still limited overall.
Emotional and Psychological Impacts
Visible skin lesions and accompanying itch or soreness often significantly detracts from emotional wellbeing and body image. Confronting public misconceptions poses an added challenge.
Seeking social support, whether from loved ones, patient advocacy groups or mental health professionals, validates experiences and fosters resilience. While symptoms wax and wane, self-care underpins the ability to cope with disease fluctuations. Partners can provide invaluable empathy and assistance with treatment.

Conclusion
In summary, psoriasis and seborrheic dermatitis are two distinct dermatologic disorders with important differences in their characteristics and management considerations.
Misdiagnosis between plaque psoriasis or scalp psoriasis and seborrheic dermatitis is common. Clinical evaluation together with skin biopsy helps distinguish ambiguous cases. Correctly delineating between these conditions ensures appropriate treatment to attain disease control and improve patient quality of life.
Lifestyle measures like stress reduction techniques, skin protection, dietary improvements and positive social support work hand-in-hand with medical therapy to help sufferers better adjust to living with chronic skin disease.
Future research elucidating the role of skin and gut microbiota in propagating inflammation will uncover additional avenues for treatment advancements.
~~~
“`
Decoding Skin Conditions: Seborrheic Dermatitis Versus Psoriasis
Are you struggling with flaky, irritated skin and unsure if it’s seborrheic dermatitis or psoriasis? These common skin conditions can look similar but have different roots and require distinct approaches to treatment. This guide will help you understand the key differences to ensure proper diagnosis and management.
Quick Article Highlights:
- Understand the core differences: Seborrheic dermatitis is a reaction to yeast, while psoriasis is an autoimmune condition.
- Recognize key symptoms: Learn to differentiate between greasy scales of seborrheic dermatitis and the silvery plaques of psoriasis.
- Identify affected areas: Note how location patterns differ between the two conditions.
- Explore treatment options: Discover the specific treatments for each condition, from topical antifungals to systemic medications.
- Minimize misdiagnosis risks: Understand why accurate diagnosis is crucial for effective management and avoiding inappropriate treatments.
Both seborrheic dermatitis and psoriasis can significantly impact your well-being if not properly addressed [1]. Knowing how to tell them apart is the first step towards clearer, healthier skin. Let’s dive into a detailed comparison.

Seborrheic Dermatitis: An In-Depth Guide
Seborrheic dermatitis is a persistent skin condition characterized by redness (erythema), scaling, and flaking [2]. It commonly targets areas rich in oil glands (sebum), such as the scalp, central face, and upper back.
Symptoms and How It Progresses
Watch out for these common signs [3]:
- Greasy, red skin covered in white or yellowish, flaky scales
- Patches of irritated, dry skin
- Itching and burning sensations
Seborrheic dermatitis typically develops gradually, and its severity can fluctuate. Stress and hormonal shifts can worsen symptoms [4]. Without treatment, symptoms tend to be long-lasting with occasional flare-ups.
Cradle cap, a common form in infants (3-4 months old), usually resolves on its own within a year [4]. However, seborrheic dermatitis often reappears around puberty and can persist into adulthood, often peaking in severity after age 50 [4].
Effective Treatment Strategies
Topical antifungal treatments are the primary approach, using agents like ketoconazole, zinc pyrithione, selenium sulfide, or salicylic acid [5]. These target Malassezia yeasts, which are believed to play a role in seborrheic dermatitis [6].
For more stubborn cases, doctors might prescribe topical corticosteroids and calcineurin inhibitors alongside antifungals. Phototherapy can also be considered. Identifying and avoiding potential dietary triggers may also help reduce flare-ups.
While seborrheic dermatitis can be effectively managed, a complete cure is often elusive [1]. Recurrences are common, particularly during times of immune system changes, stress, or hormonal fluctuations [3].
Psoriasis: An In-Depth Guide
Psoriasis is an autoimmune condition that speeds up skin cell production. This rapid turnover leads to raised, inflamed, scaly patches called plaques on the skin [7].
Symptoms and How It Progresses
Key indicators of psoriasis include [8]:
- Red, inflamed skin patches covered with scales
- Silvery-white scales or plaque buildup
- Nail changes: pitting, splitting, or loosening of nails
- Joint issues: pain, stiffness, and swelling (psoriatic arthritis)
Psoriasis typically follows a pattern of flare-ups (relapses) and periods of improvement (remissions). It’s generally a lifelong condition once diagnosed, although the course and severity can vary greatly from person to person [9].
Types of Psoriasis Explained
Psoriasis manifests in several forms:
- Plaque Psoriasis: The most prevalent type (about 90% of cases), characterized by raised, red plaques with silvery scales. Common locations include knees, elbows, scalp, and torso [10].
-
Guttate Psoriasis: Features small, droplet-shaped sores on the trunk, arms, legs, and scalp. Often triggered by bacterial throat infections and may resolve spontaneously [11].
-
Inverse (Flexural) Psoriasis: Develops smooth, red lesions in skin folds like armpits, groin, and under breasts. Lacks the typical thick scales due to moisture and friction in these areas.
-
Pustular Psoriasis: Marked by white, pus-filled blisters on red skin. Characterized by cycles of flares and can be serious if widespread, requiring immediate medical attention [12].
-
Erythrodermic Psoriasis: A severe form involving widespread inflammation and shedding of most of the skin. Can arise suddenly or from specific triggers like corticosteroid withdrawal. It’s a serious condition due to potential fluid and protein loss.
Effective Treatment Strategies
Treatment for psoriasis depends on severity.
Mild to Moderate Psoriasis: Topical treatments are usually the first line of defense:
- Corticosteroids: Potent anti-inflammatories, but long-term use can cause skin damage [13].
- Vitamin D Analogs: Help regulate skin cell growth [14].
- Tazarotene: A retinoid that reduces inflammation.
- Anthralin: Slows down skin cell turnover [15].
- Moisturizers: Essential for soothing and hydrating dry, irritated skin.
Moderate to Severe Psoriasis:
- Phototherapy: Controlled UV light exposure to reduce skin cell overproduction and inflammation [16].
- Systemic Medications: Oral or injectable drugs like methotrexate, cyclosporine, and biologics target the immune system’s role in psoriasis. These require careful monitoring due to potential side effects and organ toxicity [9].

Seborrheic Dermatitis vs. Psoriasis: Key Differences
While they may look alike, seborrheic dermatitis and psoriasis have distinct origins, patterns, and triggers.
| Feature | Seborrheic Dermatitis | Psoriasis |
|---|---|---|
| Pathogenesis (Cause) | Reaction to Malassezia yeast [6] | Autoimmune; IL-17/IL-23 pathway [7] |
| Scales | Greasy, yellowish | Thick, silvery-white, well-defined borders |
| Location | Face (center), scalp, upper back, chest; spares limbs | Knees, elbows, trunk, scalp, nails (psoriasis only), can be anywhere |
| Course | Fluctuating, periodic flares | Chronic, relapsing-remitting |
| Triggers | Sebum changes, humidity, pH, stress, immune status | Genetics + infections, meds, skin injury, stress, cold [17, 18] |
| Related Conditions | Metabolic issues, depression [1] | Psoriatic arthritis (10-30%) [19], heart risks, mental health |
| Treatment | Antifungal topicals, steroid topicals | Topicals, phototherapy, systemic drugs (methotrexate, biologics) |
| Prognosis | Persistent, manageable | Lifelong, variable course |
Scalp Issues: Spotting the Difference
Both conditions commonly affect the scalp, but there are clues to tell them apart.
Seborrheic Dermatitis of the Scalp:
- Appearance: Greasy, yellowish flakes with redness.
- Hair Impact: Hair damage is typically reversible.
- Key Features:
- Mild to moderate scales
- Common itchiness
- No permanent hair loss
- Responds to antifungal shampoos and sometimes topical steroids [2]
Scalp Psoriasis:
- Appearance: Thick, silvery plaques with sharp borders that may bleed easily.
- Hair Impact: Higher risk of hair breakage and potentially permanent hair loss.
- Key Features:
Quick Guide: Scalp Seborrheic Dermatitis vs. Scalp Psoriasis
| Feature | Seborrheic Dermatitis | Scalp Psoriasis |
|---|---|---|
| Inflammation | Milder [20] | Thicker plaques [9] |
| Scale Color/Type | Greasy, yellow | Silvery, prominent [10] |
| Scalp Area Affected | Central scalp | Any part of the scalp [8] |
| Hair Changes | Reversible | Higher risk of permanent hair loss [10] |
| Itch | Less common [2] | Frequent [9] |
| Joint Issues | No | Possible psoriatic arthritis [19] |

Risks of Misdiagnosis
It’s easy to mistake seborrheic dermatitis for scalp or plaque psoriasis, and vice versa. However, misdiagnosis can lead to ineffective treatment.
Seborrheic dermatitis, especially on the face and scalp, can be confused with psoriasis. Conversely, psoriasis on the body, particularly inverse psoriasis, can be misdiagnosed as seborrheic dermatitis due to the lack of thick plaques in skin folds.
Treating seborrheic dermatitis as psoriasis might lead to unnecessary systemic drugs or phototherapy, with potential side effects [21]. These stronger treatments won’t be effective if the problem is yeast-related, not autoimmune.
On the other hand, missing a psoriasis diagnosis delays proper immune-targeted treatment. Untreated psoriasis can worsen skin and joint damage and negatively impact mental and physical health. Accurate diagnosis of severe forms like pustular and erythrodermic psoriasis is critical due to the risk of serious complications like electrolyte imbalances [12].
A thorough medical history and physical exam are key to accurate diagnosis, focusing on symptom location, triggers, and related health issues. In unclear cases, a skin biopsy or a trial of antifungal medication may be necessary to rule out seborrheic dermatitis when psoriasis is suspected.
Living Well with Seborrheic Dermatitis and Psoriasis
Managing chronic skin conditions involves both medical treatment and lifestyle adjustments for physical and emotional well-being.
Lifestyle Tips for Symptom Relief
Consider these strategies to help manage symptoms:
- Stress Reduction: Practice relaxation, seek counseling, or join support groups to manage stress and mood.
- Gentle Skin Care: Use mild cleansers, avoid harsh fabrics like wool and synthetics, and opt for smooth materials.
- Moisturize Regularly: Apply fragrance-free moisturizers, especially ointments, after bathing to lock in hydration.
- Limit Alcohol: Alcohol can worsen inflammation and interact with psoriasis medications.
- Stop Smoking: Smoking increases the risk and severity of both conditions.
- Treat Infections Promptly: Address strep infections to prevent guttate psoriasis flares. Use antibiotics judiciously.
- Healthy Diet: Focus on an anti-inflammatory diet rich in fruits, vegetables, fiber, and omega-3s.
- Vitamin D Management: Ensure adequate vitamin D through safe sun exposure, diet, or supplements, as low levels can worsen autoimmune conditions.
- Consider Gentle Remedies: Some find relief from aloe vera, milk thistle, or curcumin, but research is still ongoing.
Emotional Well-being and Support
Visible skin issues and discomfort can impact self-esteem and emotional health. Dealing with public misunderstandings can add to the burden.
Seeking support from loved ones, patient groups, or mental health professionals can provide validation and coping strategies. Self-care and strong partnerships are essential for navigating the ups and downs of chronic skin conditions.
In Conclusion
Seborrheic dermatitis and psoriasis are distinct skin disorders requiring different management approaches.
Accurate diagnosis, especially distinguishing between seborrheic dermatitis and scalp or plaque psoriasis, is crucial. Clinical evaluation and skin biopsies can help in complex cases. Correct diagnosis ensures appropriate treatment, leading to better disease control and improved quality of life.
Combining medical treatments with lifestyle adjustments like stress management, skin care, diet, and social support empowers individuals to live more comfortably with these chronic skin conditions.
Continued research into the skin and gut microbiome promises to reveal new treatment avenues for these inflammatory conditions in the future.
No Comments
Be the first to start a conversation