- Quick Relief for Seborrheic Dermatitis: Selenium sulfide is a powerful antifungal wash-off treatment.
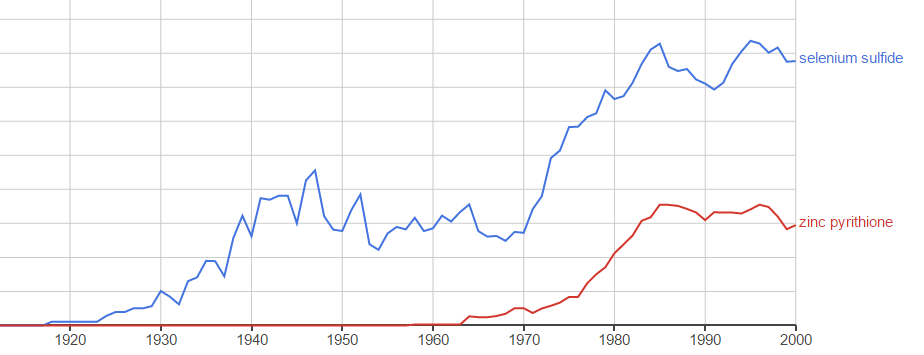
- History & Effectiveness: Initially explored as a less greasy, odorless alternative to sulfur, Selenium Sulfide has proven effective since the 1950s.
- Key Benefits: Combats Malassezia fungus, reduces skin cell turnover, and exfoliates the scalp.
- Safety Profile: Generally safe for wash-off use, with low skin absorption, but long-term safety requires consideration.
- Comparison: While effective, newer antifungals like ketoconazole may offer superior results and fewer side effects.
Selenium Sulfide for Seborrheic Dermatitis: An Effective Treatment Overview
Selenium sulfide is a common antifungal agent used to treat seborrheic dermatitis. It’s important to note that it is recommended for wash-off formulations only due to potential toxicity concerns [1]. This article explores the history, effectiveness, safety, and mechanisms of selenium sulfide in managing seborrheic dermatitis.

The Backstory of Selenium Sulfide
In the 1950s, sulfur was a leading seborrheic dermatitis treatment. Despite its effectiveness, its greasy texture and unpleasant odor often led patients to discontinue use.
Selenium, sharing chemical and physical similarities with sulfur, offered a potential alternative. Although selenium’s toxicity has been recognized since the 1840s, its resemblance to sulfur, combined with potentially better user experience, piqued researcher interest in its application for seborrheic dermatitis.
In 1951, researchers investigated selenium disulfide (selenium sulfide) for seborrheic dermatitis treatment [2].
Initial study results were encouraging.
In a study of 90 participants with seborrheic dermatitis, 73 (81.1%) achieved complete remission during treatment, with optimal results typically seen between the fourth and eighth week.
Despite its demonstrated efficacy, concerns about potential toxicity remained a focus, particularly regarding selenium absorption through the skin.
Ultimately, the balance of effectiveness and improved user experience outweighed toxicity worries. Research continued, and selenium sulfide became a popular choice in seborrheic dermatitis shampoos.

How Selenium Sulfide Works to Combat Seborrheic Dermatitis
Selenium sulfide’s effectiveness is attributed to a combination of actions:
- Antifungal Action: Targets Malassezia yeast.
- Keratinocyte Regulation: Reduces rapid skin cell growth.
- Exfoliation: Peels away the outer skin layer.
Research suggests its primary benefit comes from its antifungal activity against Malassezia yeasts [3]. However, its impact on skin cells also plays a role.
Selenium sulfide has a toxic effect on keratinocytes, the main cells of the epidermis [4]. This toxicity reduces the rate of keratinocyte division and growth. In seborrheic dermatitis, an accelerated rate of keratinocyte proliferation is considered a key factor [5]. By slowing this process, selenium sulfide can help manage the condition.
Additionally, selenium sulfide acts as a peeling agent, softening and shedding the skin’s outer layer [6]. This exfoliation helps remove the top layer of skin affected by seborrheic dermatitis, potentially speeding up recovery.

Understanding Selenium Sulfide Safety
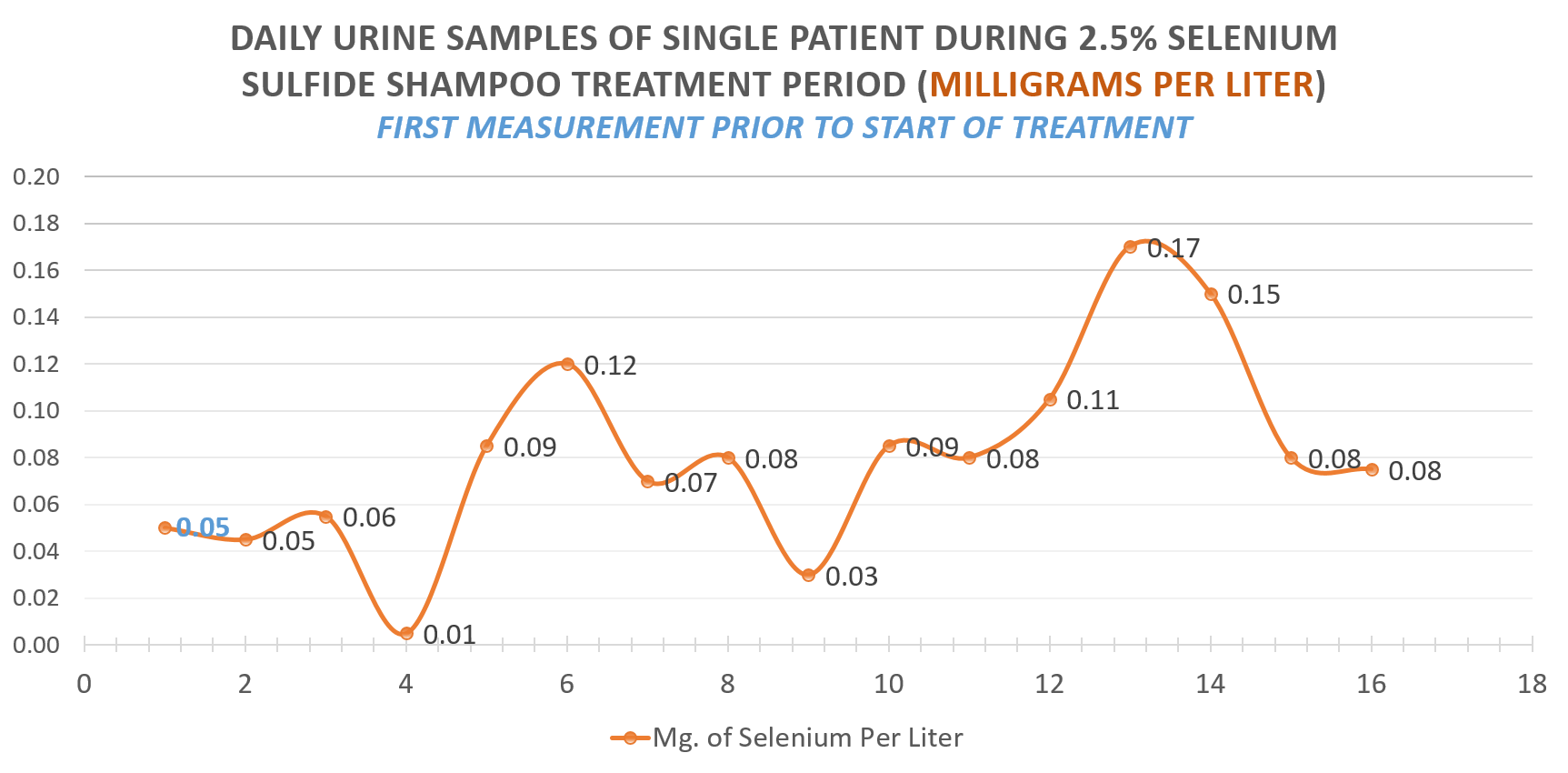
While effective, selenium sulfide does raise safety concerns due to selenium’s inherent toxicity [7]. Long-term selenium sulfide use requires careful consideration regarding potential adverse effects [8].
The general view is that selenium sulfide is among the least toxic selenium compounds. This is largely because of its low solubility in water, which limits its absorption through the skin [9].
A year-long study monitoring weekly selenium sulfide use found normal urinary selenium levels in participants [10]. This suggests minimal selenium absorption through the skin. However, this study was small, involving only 16 participants using a 1% selenium sulfide shampoo once a week.
Another study following 140 people for two years reported no toxic effects [11]. However, 31% of participants (43 individuals) experienced increased oiliness (sebaceous gland secretions) after 3-4 weeks.
Less common side effects associated with selenium sulfide include:
- Hair Loss: Diffuse hair loss with regular use [12]
- Contact Dermatitis: Skin irritation [13]
- Hair Root Issues: Abnormal hair root development with prolonged exposure [14]
Overall, selenium sulfide carries a higher potential for safety concerns and side effects compared to newer antifungal alternatives like ketoconazole, zinc pyrithione, and clotrimazole.
Selenium Sulfide Compared to Other Antifungal Treatments
Studies have compared selenium sulfide to other common antifungals:
In a study of 246 people, 2% ketoconazole outperformed 2.5% selenium sulfide [15]. All nine reported adverse events occurred in the selenium sulfide group.
Lab tests showed 2% ketoconazole to be at least ten times more effective than 1% selenium sulfide (the standard concentration) against Malassezia furfur [16].
Guinea pig studies indicated that both 2% zinc pyrithione and 2% ketoconazole had stronger antifungal activity against Malassezia than 2.5% selenium sulfide [17]. Ketoconazole demonstrated the strongest effect, while zinc pyrithione was slightly more effective than selenium sulfide.
Concentration Matters in Studies
It’s important to note that these comparative studies often use higher concentrations of antifungals than typically found in over-the-counter products.

Selenium Sulfide for Seborrheic Dermatitis: Key Takeaways
This section has provided an overview of selenium sulfide as a treatment for seborrheic dermatitis. Here are the main points:
- Selenium sulfide is a widely used seborrheic dermatitis treatment, available in wash-off formulations.
- It was developed as an alternative to sulfur, offering similar benefits without the drawbacks of greasiness and odor.
- Its primary mode of action is believed to be its antifungal effect against Malassezia yeasts.
- Additional beneficial properties include its ability to reduce keratinocyte proliferation and exfoliate the skin.
- Selenium sulfide is a known toxic substance, and long-term use raises safety considerations.
- Research suggests that selenium sulfide’s safety profile is related to its limited skin absorption, but prolonged skin contact is not advised.
- Newer antifungal treatments appear to be more effective and have a lower risk of side effects.
No Comments
Be the first to start a conversation