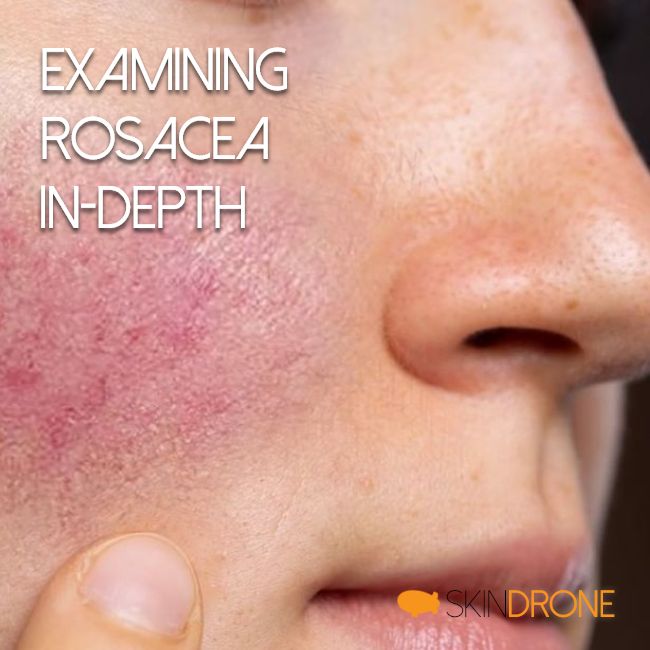
- Rosacea is a common skin condition often linked to genetics and environmental factors.
- Symptoms include facial redness, bumps, eye irritation, and visible blood vessels.
- While similar to seborrheic dermatitis, rosacea has distinct underlying causes and treatments.
- Diagnosis is based on symptoms, as there are no definitive lab tests.
- Management focuses on symptom control and trigger avoidance, with various treatments available.
Understanding Rosacea In-Depth
Rosacea is a chronic skin condition frequently observed alongside seborrheic dermatitis. While both share some symptoms, understanding their differences is key to effective management.
Genetics and family history appear to play a significant role in rosacea [], but environmental factors are equally important. Statistically, rosacea is more frequently diagnosed in women, yet it often presents more aggressively in men [1].
Like seborrheic dermatitis, rosacea tends to progress and spread if left unmanaged. Despite overlapping symptoms, their root causes and treatment strategies diverge significantly. Most practitioners focus on achieving initial symptom control followed by ongoing management rather than complete eradication.

Recognizing Primary Rosacea Symptoms
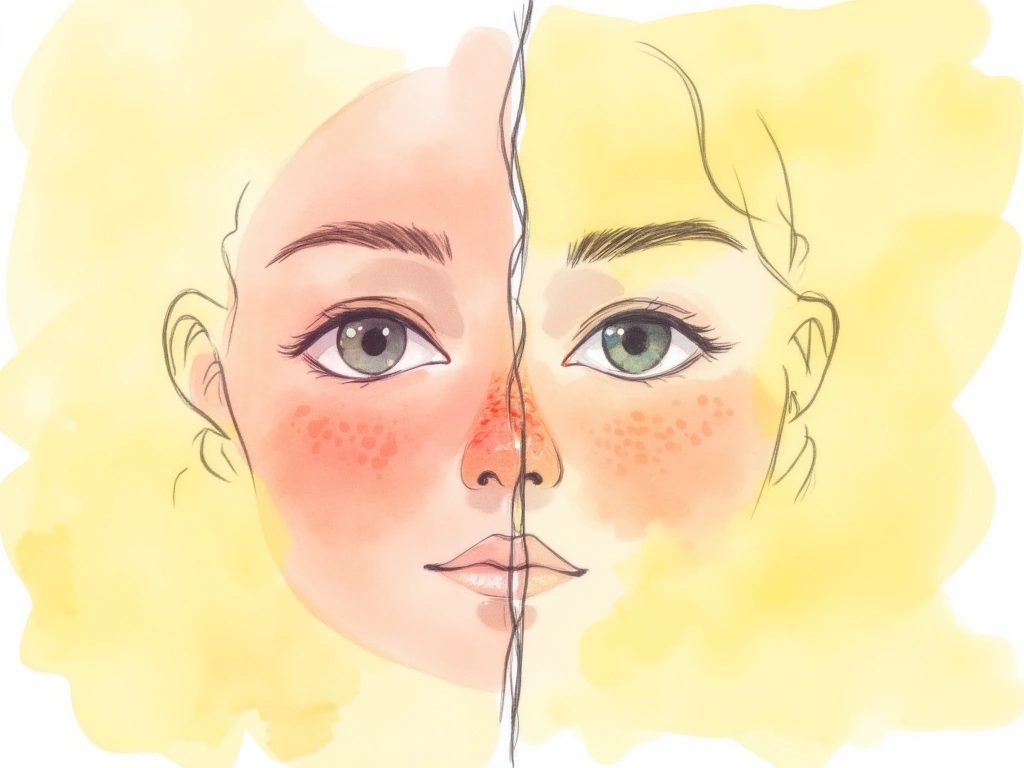
The hallmark symptoms of rosacea include [2, 3]:
- Facial Redness (Erythema): Redness in areas similar to those affected by seborrheic dermatitis.
- Swollen Red Bumps: Acne-like bumps on the skin.
- Eye Issues: Dryness, irritation, and itching affecting the eyes.
- Flushing: Sensations of heat and tingling on the skin.
- Visible Blood Vessels (Telangiectasia): Small, noticeable blood vessels on the skin surface.
- Red Nose: Characteristic redness of the nose.
- Swelling (Edema): Fluid retention causing skin swelling.
- Skin Dryness: Often a secondary symptom due to overlapping skin conditions or treatments.
A key differentiator from seborrheic dermatitis is the absence of primary skin flaking and abnormal sebum (oil) production in rosacea.
Topical Steroid Side Effects and Rosacea
It’s important to rule out topical steroid use as a cause of rosacea-like symptoms. Prolonged use of these medications can mimic rosacea [4, 5]. In such cases, symptoms are considered side effects and typically resolve after discontinuing steroid application.
Rosacea: Core Concepts
Despite extensive research, the medical community’s understanding of rosacea is still evolving. Global research on rosacea is growing, yet uncertainty persists regarding its complexities.
A significant portion of available literature may be influenced by funding from companies with vested interests in specific treatments, introducing potential biases [6]. This bias can lead to a wealth of proposed treatments without a corresponding increase in fundamental understanding of the condition itself.
Diagnosing Rosacea
Currently, no standardized lab tests exist to definitively diagnose rosacea [6]. Diagnosis primarily relies on a healthcare professional’s expertise in recognizing common rosacea symptoms and subtypes, and differentiating them from similar conditions.
Accurate diagnosis involves not just identifying rosacea, but also pinpointing the specific subtype. Subtype identification is crucial for tailoring effective treatment strategies [7].
For instance, individuals experiencing mainly facial flushing, skin sensitivity, and redness often react poorly to many topical treatments. Conversely, those with bumps/pimples (pustules/papules), increased oil production, and a butterfly-pattern redness tend to tolerate topical treatments better.
Four Rosacea Subtypes
Initially, rosacea was categorized into two main types: one characterized by redness and flushing, and another by papules and pustules. Currently, four distinct subtypes are recognized:
- Erythematotelangiectatic Rosacea: Characterized by skin flushing, persistent redness in specific areas, and potentially prominent blood vessels.
- Papulopustular Rosacea: Features the symptoms of the erythematotelangiectatic subtype, along with small bumps and papules.
- Phymatous Rosacea: Involves skin thickening and swelling, particularly affecting the nose (rhinophyma), chin, forehead, cheeks, and ears.
- Ocular Rosacea: Manifests as chronic eye irritation with symptoms like burning, stinging, dryness, itching, light sensitivity, and redness.

Potential Rosacea Causes
The exact cause of rosacea remains unclear, and no single consensus has been reached. However, current research points to several contributing factors:
- Vascular Abnormalities: Irregularities in facial blood flow are evident [8] and may be linked to hormonal imbalances, specifically vasoactive intestinal peptide [9], gastrin [10, 11], serotonin, and histamine [12]).
- Altered Innate Immunity: The skin’s defense system uses antimicrobial peptides to combat infection and injury [13]. These peptides also mediate cellular communication and inflammation. Elevated levels of cathelicidins (an antimicrobial peptide) in rosacea-affected skin suggest an abnormal immune response [14, 15, 16].
- Climactic Exposures: Prolonged skin exposure to environmental stressors like high heat or UV radiation can chronically damage facial blood vessels and connective tissues [8, 17, 18].
- Dermal Matrix Degeneration: Issues within blood vessel linings [18, 19] and/or compromised connective tissues [20, 21] may lead to structural skin changes, increased vessel permeability, and localized pooling of blood, inflammatory agents, and metabolic waste.
- Dietary and Chemical Triggers: Spicy foods, alcohol, and hot drinks are known rosacea flush triggers (not causes) [22, 23]. Certain medications, including topical/nasal steroids, nicotinic acid, and high-dose vitamin B6, can induce flushing or rosacea-like symptoms [5, 24, 25, 26, 27, 28].
- Pilosebaceous Unit Abnormalities: Structural irregularities in the pilosebaceous unit [21, 29] (hair follicle, hair, arrector pili muscles, and sebaceous gland) may increase infiltration by inflammatory cells (neutrophils, eosinophils, lymphocytes, plasmacytes, macrophages, mast cells) and external antigens (Propionibacterium acnes and Demodex mites).
- Demodex Mite Infestation: Overpopulation of Demodex mites in hair follicles (mites naturally present on skin) may contribute to rosacea progression [30, 31]. However, the exact role remains debated [21, 29], as improvement can occur without reducing mite counts [32, 33].
- Helicobacter Pylori Infection: A possible link between rosacea and gastrointestinal issues [34] has raised suspicion that Helicobacter pylori infection could be a cause in some cases [35, 36, 37]. Studies on H. pylori eradication have yielded mixed results [38, 39, 40], and some suggest the overall effect of antibiotics, rather than specifically H. pylori elimination, may be responsible for improvements [41, 42].
The persistent uncertainty surrounding rosacea’s causes may stem from unidentified factors or individual variations among sufferers. Future research and technologies may provide clearer insights.
Rosacea Treatment Strategies
Given rosacea’s complex nature, no single treatment guarantees complete symptom resolution. Much of the literature suggests rosacea is a chronic condition requiring ongoing management. However, this remains debated, and evolving knowledge may change this perspective.
Regardless of the long-term outlook, understanding common treatment approaches can offer valuable insights and potential relief.
Common rosacea treatments include:
- Trigger avoidance (diet, environment, medications, etc.)
- Systemic antibiotics (tetracycline or metronidazole)
- Isotretinoin
- Topical antibiotics (metronidazole, clindamycin phosphate, permethrin)
- Topical retinoids and precursors (tretinoin or retinaldehyde)
- Sulfur (with or without sodium sulfacetamide)
- Azelaic acid
Many treatments are effective for specific symptoms (e.g., redness or pustules/papules), and combination therapies are frequently used.
Trigger Avoidance
Early in rosacea management, identifying and minimizing triggers can effectively reduce overall symptom severity, particularly skin redness [43, 44].
Common rosacea triggers include [44]:
- Foods:
- Liver and smoked meats
- Yogurt, sour cream, hard cheeses (excluding cottage cheese)
- Avocados, bananas, red plums, raisins, figs, citrus fruits
- Eggplant, tomatoes, spinach, lima beans, navy beans, peas
- Chocolate and vanilla
- Soy sauce and vinegar
- Hot and spicy foods
- High-yeast foods
- Beverages:
- Alcoholic beverages, especially red wine
- Hot drinks
- Stress and Anxiety
- Environmental Factors:
- Sun exposure
- Strong winds
- Extreme humidity (high or low)
- Temperature extremes (hot or cold)
- Skincare Products:
- Alcohol, witch hazel, fragrances, menthol, eucalyptus oil, clove oil, peppermint, sodium lauryl sulfate
- Harsh cleansers (e.g., bar soap)
- Over-washing
- Aggressive exfoliation
- Medications:
- Vasodilators
- Topical steroids
- Medical Conditions:
- Menopause
- Caffeine withdrawal
- Chronic cough
- Excessive Physical Exertion
Identifying personal triggers often requires trial and error. It’s crucial to maintain a pragmatic approach and avoid impulsive treatment changes, as stress from constant switching can itself exacerbate rosacea.
Systemic Antibiotics
Metronidazole and tetracycline have long been used to treat rosacea [45, 46]. Doxycycline is currently the only FDA-approved tetracycline for rosacea [47, 48].
Long-term systemic antibiotic use is limited by potential complications [49, 50, 51, 52] (especially with tetracyclines) and relapse risk after treatment ends [53].
Oral antibiotics primarily target pustules and papules, with less impact on redness (erythema). Careful risk-benefit assessment with a healthcare professional is essential before starting systemic antibiotics.
Antibacterial vs. Anti-inflammatory Effects
The anti-inflammatory properties of antibiotics may be more significant for rosacea symptom reduction than their antibacterial actions [54, 48].
Isotretinoin
Isotretinoin, a synthetic retinoid related to retinol, is a common acne treatment that is also effective for rosacea [55, 56]. It notably improves papules and pustules [57] and reduces redness [58, 59].
However, isotretinoin intolerance and side effects are common, including mucosal dryness, lip inflammation (cheilitis), skin inflammation (dermatitis), muscle/joint pain, headaches, and elevated triglycerides [60, 61].
Topical Antibiotics
Topical antibiotics minimize systemic side effects by targeting application to affected areas. However, antibiotic resistance remains a potential concern [62, 63].
Metronidazole and tetracycline are frequently used topical options [64, 65] in creams, lotions, and gels. Clindamycin phosphate and permethrin are also used topically.
Topical Retinoids and Retinoid Precursors
Inspired by isotretinoin’s efficacy, topical approaches using retinoids have been explored.
Tretinoin, another retinoic acid for acne, shows promise for rosacea. Topical tretinoin was comparable to systemic isotretinoin in reducing both papules/pustules and redness [66]. However, adverse reactions are common [67, 68].
Retinaldehyde, a natural retinol precursor, requires skin conversion to retinoic acid or retinal [69]. Studies suggest retinaldehyde is better tolerated than tretinoin [70] and effectively reduces rosacea-related redness [71].
Sulfur
Sulfur is a more natural topical rosacea treatment. Some studies suggest it has similar efficacy to antibiotics in symptom reduction, potentially with fewer long-term side effects [72].
A common complaint is sulfur’s distinct odor, which can linger after washing.
Combining sulfur with sodium sulfacetamide (which also has anti-inflammatory and antibacterial properties [73]) may enhance effectiveness and reduce the required sulfur concentration [74]. However, some may prefer sulfur alone to minimize potential adverse reactions.
Azelaic Acid
Azelaic acid, another acne treatment, is also effective for rosacea. Some studies suggest it’s a viable alternative to topical metronidazole [75].
Benefits include its natural origin and reduced risk of long-term side effects [76].
Interestingly, azelaic acid is produced by Malassezia furfur, a yeast implicated in seborrheic dermatitis [77], yet topical azelaic acid improves seborrheic dermatitis symptoms [78].
Exploring Natural Rosacea Treatments
Due to inconsistent results and concerns about side effects with conventional treatments, interest in natural alternatives is growing.
Based on current research, two natural approaches show particular promise:
- Niacinamide and Zinc Supplementation: A supplement containing 750mg nicotinamide, 25mg zinc, 1.5mg copper, and 500mcg folic acid daily showed rosacea improvements comparable to oral antibiotics [79]. This is attributed to anti-inflammatory, bacteriostatic, and sebum-reducing properties [80].
- Licorice Extract: Licorice, known for its anti-inflammatory properties, has historical medicinal use. Topical ointments with specific licorice extracts have significantly reduced redness and inflammation in mild rosacea [81], atopic dermatitis [82], and UV-induced redness [83].
Other natural approaches with potential benefits based on their skin-healing and anti-inflammatory properties [84, 85, 86] include:
- Green tea washes and extracts
- Topical aloe vera
- Topical chamomile
- Turmeric supplements
- Mushroom extracts
- Probiotics
- Omega-3 fatty acids
While anecdotal reports of effectiveness exist for these, specific research on their use in rosacea is still limited.

Rosacea: Key Takeaways
This article provides a detailed overview of rosacea and its relationship to seborrheic dermatitis. While many questions remain unanswered, this information serves as a helpful starting point for those affected by rosacea.
- Rosacea is an inflammatory skin condition primarily affecting the face, often localized to specific areas, and with a likely genetic component.
- Rosacea frequently co-occurs with seborrheic dermatitis, but they are distinct conditions, primarily differing in sebum’s role.
- Rosacea is classified into four subtypes, and accurate subtyping is crucial for targeted treatment selection.
- Potential rosacea causes include blood flow irregularities, immune system dysfunction, UV damage, skin structure changes, Demodex mites, digestive issues, and dietary factors.
- Prolonged steroid use can mimic rosacea symptoms; steroid cessation usually leads to symptom improvement in these cases.
- Despite extensive research, a definitive single cause remains elusive, possibly due to individual variations among rosacea sufferers.
- Common treatments include trigger avoidance (diet, stress, medications), topical and systemic antibiotics, and immune-modulating agents.
- Natural treatment options like sulfur, azelaic acid, niacinamide/zinc supplements, and licorice extract ointments may be considered.
No Comments
Be the first to start a conversation