- Plaque psoriasis is an autoimmune condition, while seborrheic dermatitis is linked to a common fungus.
- Psoriasis often presents as thick, silvery scales, whereas seborrheic dermatitis is typically greasy and flaky.
- Accurate diagnosis is essential because treatments vary significantly between the two conditions.
Plaque psoriasis and seborrheic dermatitis are often confused, especially on the scalp. Psoriasis is autoimmune with thick, silvery scales, while seborrheic dermatitis is fungal-related with greasy flakes. Correct diagnosis is key for effective treatment.
Understanding Plaque Psoriasis and Seborrheic Dermatitis
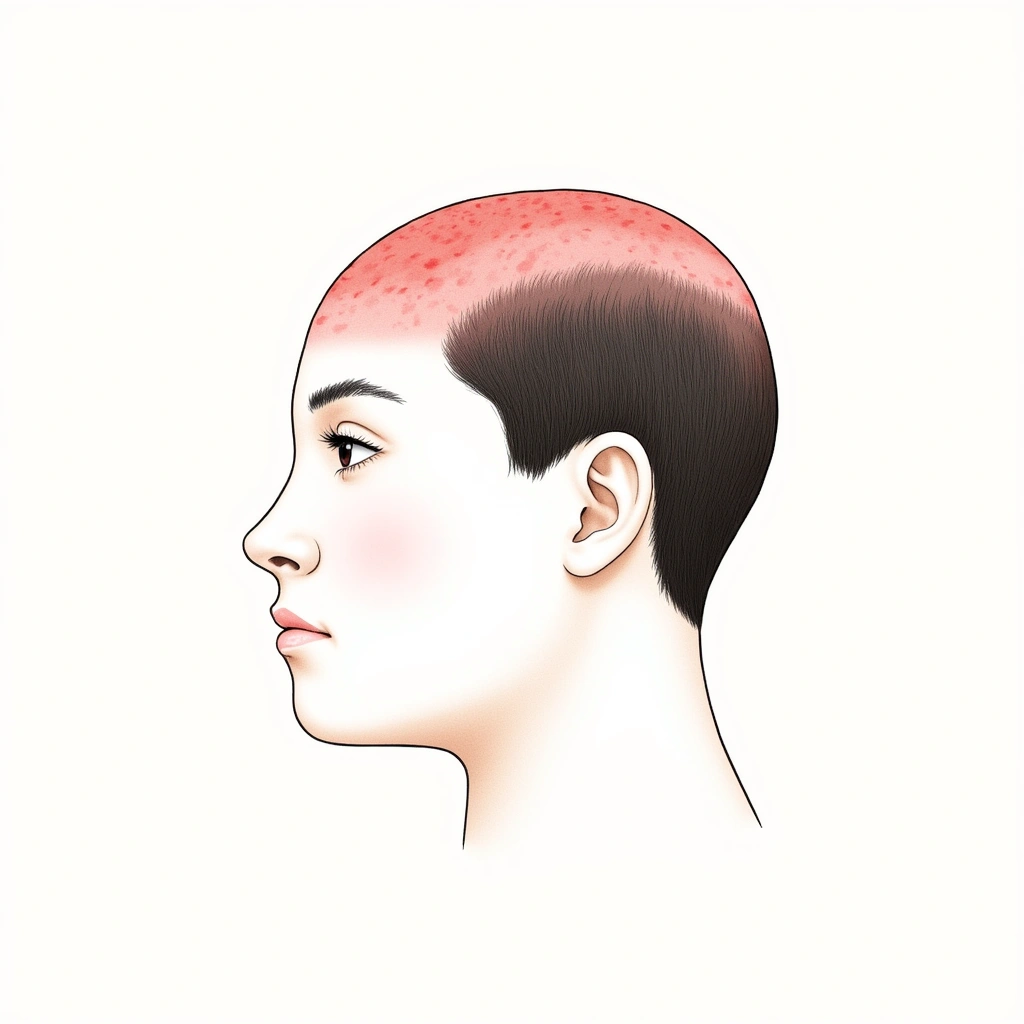
Plaque psoriasis and seborrheic dermatitis are frequent skin issues that can look alike, particularly when affecting the scalp. Both conditions can cause red, scaly patches, making it tricky to tell them apart. Knowing the differences is important because they have different causes and need different treatments. Misdiagnosis can lead to treatments that don’t work, so getting it right is key.
How Common Are They?
Plaque psoriasis affects around 3% of adults in the United States [1], which translates to over 7.5 million people. Globally, it’s also quite common, especially in Western Europe and North America [4].
Seborrheic dermatitis is even more widespread, affecting about 4.38% of people worldwide [7]. It’s more common in adults (5.64%) than children (3.70%) or newborns (0.23%), and its prevalence varies across different regions. These numbers highlight that both conditions are significant health concerns.
What Causes These Skin Conditions?
While they may look similar, plaque psoriasis and seborrheic dermatitis have different root causes.
Plaque Psoriasis: An Autoimmune Issue
Plaque psoriasis is considered an autoimmune disease. This means the body’s immune system mistakenly attacks healthy skin cells, causing them to grow too quickly. This rapid growth leads to the buildup of skin cells on the surface, forming the characteristic plaques. Key factors in psoriasis include:
- Immune System: Specifically, T-cells play a major role, and substances called cytokines (like TNF-α and IL-17) are involved in the inflammation process [3].
- Genetics: Genes play a significant role, with specific genes like HLA-Cw6 being strongly linked to psoriasis, especially when it starts at a younger age [3].
- Triggers: Certain triggers can cause psoriasis flare-ups, such as skin injury (Koebner phenomenon), infections, and certain medications [6].
Seborrheic Dermatitis: Linked to a Fungus
Seborrheic dermatitis, on the other hand, is linked to a fungus called Malassezia, which is normally found on the skin [5]. It’s not a fungal infection in the typical sense, but rather an inflammatory reaction to this fungus. Key points about seborrheic dermatitis include:
- Malassezia Fungus: An overgrowth of Malassezia is thought to irritate the skin. Specific species like M. restricta and M. globosa might be more involved [5].
- Immune Response: The body’s immune system reacts to the Malassezia fungus, leading to inflammation.
- Sebum (Skin Oil): Seborrheic dermatitis occurs in areas with many oil glands, suggesting sebum plays a role.
- Risk Factors: Conditions that weaken the immune system or neurological diseases can increase the risk, but it’s not directly caused by poor hygiene [8].

How Do They Look and Feel?
Plaque psoriasis and seborrheic dermatitis have distinct appearances and symptoms.
Plaque Psoriasis: Thick, Red, and Scaly
Plaque psoriasis is often characterized by:
- Plaques: Raised, red patches of skin.
- Scales: Thick, silvery-white scales covering the plaques.
- Location: Commonly found on elbows, knees, scalp, and lower back, often on the outer (extensor) surfaces [5]. Scalp psoriasis can extend beyond the hairline.
- Itching and Pain: Plaques can be itchy and sometimes painful.
- Auspitz Sign: Removing a scale may cause pinpoint bleeding [5].
- Nail Changes: Psoriasis can affect nails, causing pitting, separation from the nail bed (onycholysis), or thickening [2].
- Psoriatic Arthritis: About 30% of people with psoriasis may also develop joint problems [2].
User experiences highlight the severity of scalp psoriasis, with descriptions like “thick layers of dandruff” that bleed when picked, and flakes that are likened to “snowfall” [39]. Flare-ups can be triggered by stress, infections, alcohol, and even hot showers [116].
Seborrheic Dermatitis: Greasy, Flaky, and Yellowish
Seborrheic dermatitis typically presents as:
- Patches: Flaky, scaly patches that can be greasy.
- Scales: Scales are often yellowish or brownish and oily.
- Location: Found in areas rich in oil glands (seborrheic areas) such as the scalp (common cause of dandruff), face (especially nasolabial folds and eyebrows), ears, and upper chest [6].
- Itching: Mild itching is common.
- Infants: In babies, it’s known as cradle cap and usually resolves on its own [8].
- Chronic Course: In adults, it tends to be a long-term, recurring condition [8].
User accounts describe seborrheic dermatitis flakes as “oily, yellow-tinged” with itching and burning [13]. Facial redness can feel like a “permanent sunburn” [28]. Triggers include humidity, harsh hair products, and stress [714].

How Are They Diagnosed?
Distinguishing between plaque psoriasis and seborrheic dermatitis can be challenging, especially when they occur on the scalp. Doctors use several methods to diagnose these conditions.
Clinical Examination
Often, a doctor can diagnose based on the appearance and location of the skin patches. However, because they can look similar, especially on the scalp, further investigation might be needed.
Histopathology: Looking at Skin Under a Microscope
In cases where it’s hard to tell the difference, a skin biopsy may be performed. This involves taking a small sample of skin and examining it under a microscope. Histopathology can reveal key differences between psoriasis and seborrheic dermatitis at a cellular level [9].
Key Microscopic Features:
| Feature | Psoriasis | Seborrheic Dermatitis |
|---|---|---|
| Parakeratosis with Neutrophils | Very Common (100%) | Common (50%) |
| Spongiform Micropustules of Kogoj | Common (33%) | Absent (0%) |
| Clubbed Rete Ridges | Very Common (100%) | Rare (10%) |
| Follicular Plugging | Less Common (27%) | Common (70%) |
| Shoulder Parakeratosis | Rare (7%) | Common (40%) |
| Lymphocytic Exocytosis (moderate) | Rare (7%) | Common (45%) |
Psoriasis tends to show features like mounds of parakeratosis with neutrophils, spongiform micropustules of Kogoj, and clubbed rete ridges. Seborrheic dermatitis is more likely to have follicular plugging, shoulder parakeratosis, and lymphocytic exocytosis [9].
Differential Diagnosis: Ruling Out Other Conditions
It’s also important to rule out other conditions that can mimic psoriasis and seborrheic dermatitis, such as:
- Sebopsoriasis: A condition with overlapping features of both psoriasis and seborrheic dermatitis, making diagnosis more complex.
- Lichen planopilaris: Affects hair follicles and can cause scarring hair loss.
- Tinea capitis: A fungal infection of the scalp that can cause scaling and hair loss.
- Atopic dermatitis (eczema): Characterized by itchy, red patches.
- Contact dermatitis: A reaction to allergens or irritants.
- Lupus erythematosus and dermatomyositis: Other skin conditions that can affect the trunk [10].
A comprehensive clinical evaluation is necessary to consider these possibilities and reach an accurate diagnosis [10].
Treatment Approaches: How Do They Differ?
Because plaque psoriasis and seborrheic dermatitis have different causes, their treatments also differ significantly.
Plaque Psoriasis Treatments: Targeting the Immune System
Treatment for plaque psoriasis aims to slow down skin cell growth and reduce inflammation. Common approaches include:
- Topical Corticosteroids: Creams and ointments to reduce inflammation [11].
- Vitamin D Analogs: Medications like calcipotriol to slow skin cell growth [11].
- Topical Retinoids: To normalize skin cell growth [11].
- Phototherapy (UVB): Using ultraviolet light to slow skin cell growth [11]. User experiences highlight UVB phototherapy combined with high-dose vitamin D as effective [16].
- Systemic Medications: For more severe cases, medications that work throughout the body may be used [11]. These include:
Treatment often follows a step-by-step approach, starting with topical treatments and moving to stronger therapies if needed [12].
Seborrheic Dermatitis Treatments: Targeting the Fungus
Seborrheic dermatitis treatment focuses on controlling the Malassezia fungus and reducing inflammation. Common treatments include:
- Antifungal Shampoos: Shampoos containing ketoconazole, selenium sulfide, or zinc pyrithione to reduce fungal overgrowth [1314].
- Topical Corticosteroids: To reduce inflammation, especially on the face [1314].
- Oral Antifungals: In severe cases, medications like itraconazole may be considered [1314].
- Novel Topicals: Roflumilast cream (Zoryve) is a newer option showing promise [512].
User anecdotes suggest some unconventional remedies may also help with seborrheic dermatitis. Saltwater rinses and MCT oil are mentioned as potentially beneficial by some individuals [6917].
Anecdotal Insights: User Experiences and Nuances
Personal stories from individuals managing these conditions reveal important nuances beyond medical literature. Users often experience diagnostic confusion, with misdiagnosis being a common issue [314]. The emotional and social impact of both conditions is significant, affecting self-esteem and social interactions [1283].
Lifestyle modifications are frequently mentioned by users as important complementary strategies. These include:
- Stress reduction: Meditation and stress management techniques [1].
- Dietary changes: Reducing sugar and processed foods, adopting anti-inflammatory diets [16].
- Avoiding triggers: Identifying and avoiding personal triggers like alcohol, harsh products, or hot showers [171614].
Online communities, like Reddit, offer valuable peer support and information exchange for those living with these chronic skin conditions [16].
Conclusion and Key Takeaways
Distinguishing between plaque psoriasis and seborrheic dermatitis is crucial for effective treatment and management. While they may share some visual similarities, especially on the scalp, their underlying causes and appropriate treatments are different. Accurate diagnosis, considering both clinical appearance and sometimes histopathology, is essential.
- Psoriasis is an autoimmune disease, while seborrheic dermatitis is linked to a fungal response. This fundamental difference dictates treatment strategies.
- Psoriasis typically presents with thick, silvery scales on red plaques, often on elbows and knees. Seborrheic dermatitis is characterized by greasy, yellowish flakes in oily areas.
- Histopathology can be a valuable tool in differentiating the two when clinical presentation is unclear.
- Psoriasis treatment often requires stronger, immune-targeting therapies, including biologics. Seborrheic dermatitis is primarily managed with antifungal treatments.
- User experiences highlight the psychosocial impact of both conditions and the importance of lifestyle adjustments and community support in managing these chronic skin issues.
No Comments
Be the first to start a conversation