Malassezia Folliculitis: What You Need to Know
Malassezia folliculitis is a common skin condition caused by a yeast overgrowth in hair follicles. Often mistaken for acne, it’s important to understand what it is and how to treat it correctly. This guide breaks down the key aspects of Malassezia folliculitis, drawing from the latest research and real-world experiences.
- Learn what Malassezia folliculitis is and why it’s often confused with acne.
- Discover effective treatments, from topical creams to oral medications.
- Understand how user experiences can offer valuable insights into managing this condition.
Malassezia folliculitis is a yeast infection of the hair follicles that looks like acne but needs different treatment. This article will explain how to identify and manage it effectively.
Understanding Malassezia Folliculitis
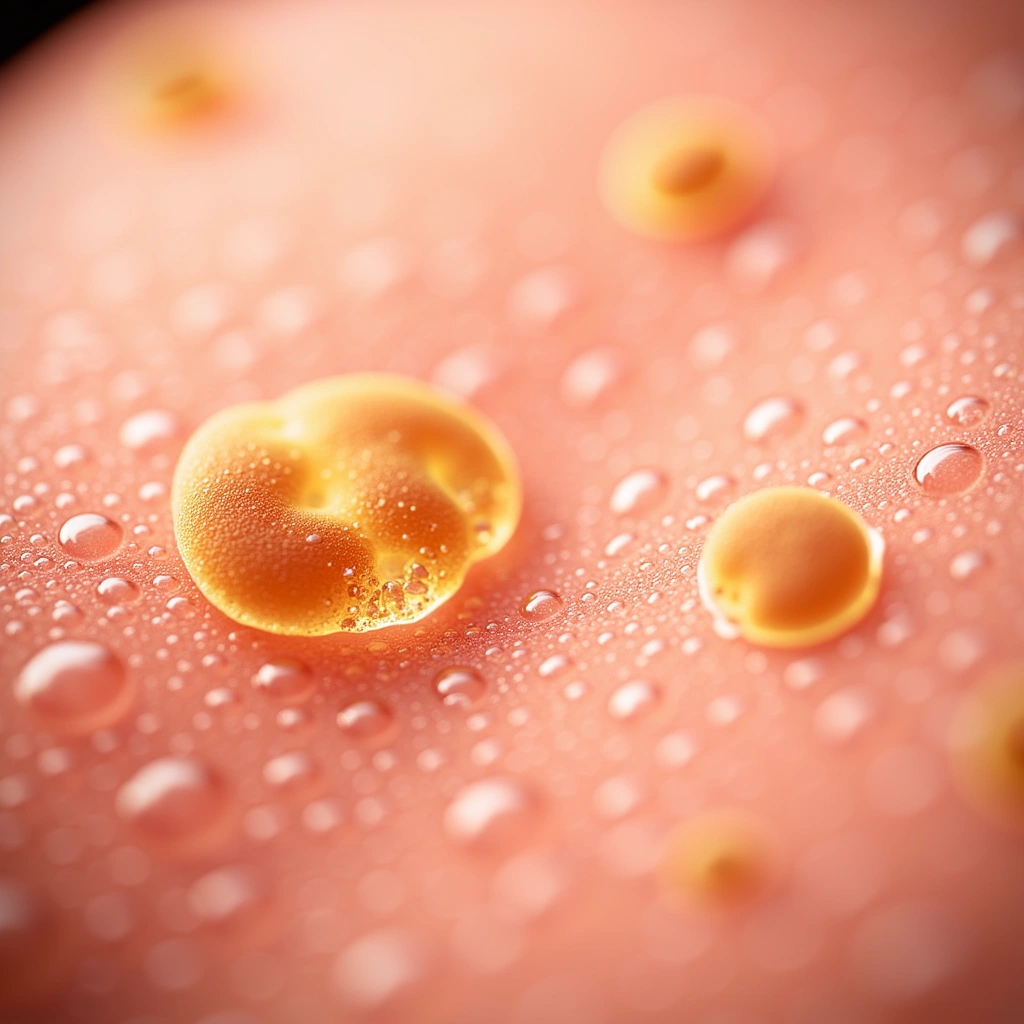
Malassezia folliculitis, also known as Pityrosporum folliculitis or sometimes “fungal acne,” is caused by an overgrowth of Malassezia yeast. These yeasts, including species like M. globosa, M. sympodialis, and M. restricta, are normally found on your skin [1]. However, under certain conditions, such as a weakened immune system, antibiotic use, or hot, humid weather, these yeasts can multiply and cause infection [2].
This condition typically shows up as small, itchy bumps or pus-filled spots that look similar to acne. It’s more common in teens and young adult men and often appears on the upper back and chest [3].

Diagnosing Malassezia Folliculitis
One of the biggest challenges with Malassezia folliculitis is getting the right diagnosis. Because it looks so much like acne or bacterial folliculitis, it’s often misdiagnosed [2, 4].
What to look for:
- Itchy bumps: Malassezia folliculitis is typically itchy, unlike typical acne.
- Uniform appearance: The bumps tend to be all the same size and shape.
- Location: Commonly found on the chest, back, shoulders, and sometimes the face, neck, and upper arms [2].
To confirm a diagnosis, doctors may use lab tests such as skin scrapings, tape strips, swabs, or biopsies to look for Malassezia yeast [3]. A simple test called potassium hydroxide (KOH) preparation can help identify the yeast under a microscope [5]. This is important to distinguish it from bacterial infections which require different treatments.
Effective Treatment Options
Treatment for Malassezia folliculitis focuses on antifungal medications. The approach often depends on your overall health and how severe the condition is [3].
Topical Treatments for Mild Cases
For most people with healthy immune systems, topical antifungal treatments are usually the first step [5]. These are applied directly to the skin and are effective for mild to moderate cases. The European Academy of Dermatology and Venereology (EADV) recommends the following topical options [3]:
- Azoles: Creams like ketoconazole, miconazole, or econazole, applied 1-2 times daily for 2-4 weeks.
- Selenium sulfide: Shampoos or washes applied daily for 3 days, then weekly to maintain results.
- Ciclopirox: Available as gel, cream, or shampoo, used twice daily for 2-4 weeks.
- Propylene glycol: A 50% solution in water, applied twice daily for 3 weeks.
- Zinc pyrithione: Creams or washes, applied 1-2 times daily for 2-4 weeks.
Oral Medications for Severe or Widespread Cases
For more severe cases, or if you have a weakened immune system, oral antifungal medications might be necessary [5]. Oral treatments are also considered when topical treatments haven’t been effective. Recommended oral options include [3]:
- Itraconazole: 100-200 mg daily for 1-4 weeks.
- Fluconazole: 100-200 mg daily for 2-3 weeks or 300 mg weekly for 3 weeks.
- Ketoconazole: 200 mg daily for 2-4 weeks, but less preferred due to potential liver and heart rhythm issues.
Studies have shown that these treatments are highly effective. For example, one study showed that itraconazole significantly improved symptoms in over 84% of patients within just 7 days [6].
Important Note for Liver Health
If you have liver disease, treatment is generally the same as for those with healthy immune systems. However, oral azole medications should be used cautiously, and your liver function should be checked regularly to avoid any liver damage [3].
User Experiences and Practical Tips
Beyond medical guidelines, real-world experiences from people who have dealt with Malassezia folliculitis offer valuable insights. Online communities and personal accounts reveal common challenges and effective strategies.
Common User-Reported Issues:
- Misdiagnosis: Many users initially received incorrect diagnoses, often being told they had bacterial folliculitis or regular acne, leading to ineffective antibiotic treatments [7, 8]. Antibiotics can actually worsen Malassezia folliculitis by killing off bacteria that compete with the yeast [7].
- Self-Diagnosis: Frustrated with misdiagnoses, many people turned to online resources to identify their condition, often finding information on blogs like Simple Skincare Science [7, 9, 10].
User-Recommended Treatments and Skincare Adjustments:
- Topical Antifungals: Nizoral (ketoconazole shampoo) was frequently mentioned as a highly effective treatment when used as a leave-on mask [10]. Zinc pyrithione soaps and sulfur-based products were also helpful [9, 11].
- Skincare Modifications: Users emphasized avoiding oil-rich skincare products that can feed Malassezia yeast. Coconut oil, olive oil, and silicone-based products were often linked to flare-ups [7, 12]. Switching to “fungal acne-safe” moisturizers with ingredients like squalane oil was beneficial [9, 13]. Low pH cleansers were also recommended [8, 14].
- Adjunctive Therapies: Benzoyl peroxide and chlorhexidine washes were used by some users for their anti-inflammatory and antimicrobial properties, especially for scalp issues [15, 16].
Distinguishing Malassezia Folliculitis from Other Conditions
It’s crucial to differentiate Malassezia folliculitis from similar skin conditions to ensure correct treatment [4]. Here’s a quick comparison:
| Condition | Cause | Treatment | Key Differences |
|---|---|---|---|
| Malassezia Folliculitis | Malassezia yeasts | Antifungals (topical/oral) | Itchy, uniform bumps, responds to antifungals |
| Seborrheic Dermatitis | Malassezia yeasts | Antifungals | Scalp, face, scaling, less follicular |
| Pityriasis Versicolor | Malassezia yeasts | Antifungals | Patches of discolored skin (hypopigmented), not follicular |
| Bacterial Folliculitis | Bacteria | Antibiotics | Responds to antibiotics, not antifungals |
| Acne Vulgaris | Bacteria, oil, hormones | Antibiotics, retinoids, benzoyl peroxide | Comedones (blackheads/whiteheads), less itchy, varied lesions |

Recurrence and Long-Term Management
Unfortunately, recurrence of Malassezia folliculitis is common, with some studies reporting rates as high as 50% [2]. Therefore, maintenance therapy is often needed to prevent flare-ups [3].
Strategies for Prevention:
- Maintenance Antifungals: Weekly use of topical ketoconazole or selenium sulfide can help prevent yeast overgrowth [3].
- Product Rotation: Alternating different types of treatments like sulfur masks, salicylic acid, and azelaic acid may help prevent the yeast from becoming resistant to one treatment [9, 11].
- Environmental Factors: Regularly changing pillowcases and using antifungal laundry additives can reduce yeast exposure and reinfection [15].

Emerging and Alternative Treatments
For difficult-to-treat cases, some research is exploring alternative therapies. Photodynamic therapy (PDT) is one such option that has shown promise in small studies for recalcitrant Malassezia folliculitis [6]. However, more research is needed to fully understand its effectiveness.
It’s worth noting that while some non-academic sources suggest natural remedies like tea tree oil, these are not supported by strong scientific evidence and are not recommended in medical guidelines [17].

Conclusion and Key Takeaways
Malassezia folliculitis is a frustrating condition, often mistaken for acne, but it can be effectively managed with antifungal treatments. Topical options are usually the first line of defense for most people, while oral medications are reserved for more severe cases or those with weakened immune systems [3]. Due to high recurrence rates, maintenance strategies are essential [2]. User experiences highlight the importance of correct diagnosis, appropriate skincare, and persistence in finding the right treatment approach.
- Malassezia folliculitis is a yeast infection, not bacterial acne, and requires antifungal treatment.
- Topical antifungals are usually effective for mild cases, while oral medications are for severe or recurrent cases.
- Accurate diagnosis is crucial to avoid ineffective treatments like antibiotics.
- Modifying skincare to avoid oil-rich products can help manage and prevent flare-ups.
- Maintenance therapy is often necessary to prevent recurrence.
No Comments
Be the first to start a conversation