- Acne affects up to 90% of adolescents: Learn why it’s so common and what factors contribute.
- More than just skin deep: Understand the significant psychological impact of acne and why holistic treatment is important.
- Tailored treatments for every severity: Discover the range of acne treatments, from mild to severe cases.
- Acne vs. Seborrheic Dermatitis: Know the key differences between these often-confused skin conditions.
Acne vulgaris is an incredibly common skin condition, affecting as many as 90% of adolescents and frequently continuing into adulthood [1]. This article offers a detailed exploration of acne, covering its complex origins, how it appears clinically, treatment options based on severity, and its relationship to and differences from seborrheic dermatitis.
Understanding Acne Vulgaris: The Complex Causes
Acne develops due to a mix of interconnected factors that lead to inflammation in hair follicles and sebaceous glands [2]. Key contributors include:
- Excess sebum (oil) production
- Abnormal skin cell shedding (keratinization)
- Changes in skin bacteria
- Immune system activation
Let’s break down these factors:
The Role of Sebum
Excess sebum production is a primary starting point in acne development. Hormones, especially androgens like testosterone, increase oil gland activity, particularly during puberty. This excess oil mixes with dead skin cells inside hair follicles, creating a blockage known as a microcomedone. This trapped mixture provides a perfect environment for bacteria to thrive.
Cutibacterium acnes and Inflammation
Cutibacterium acnes (C. acnes), a common skin bacterium, flourishes within these microcomedones. It triggers inflammation through several mechanisms [3], such as:
- Attracting immune cells like neutrophils
- Boosting the production of pro-inflammatory cytokines
- Producing inflammatory free fatty acids
Inflammation is the result of the immune system reacting to C. acnes, sebum, and other irritants. This inflammatory response leads to the visible signs of acne: papules, pustules, nodules, and cysts. Acne is now recognized as primarily an inflammatory condition.
Abnormal Keratinization
Abnormal keratinization, or the excessive shedding of skin cells within the follicles, also contributes to acne. This process increases the formation of microcomedones, further exacerbating the condition.
Other Factors Worsening Acne
Several other factors can worsen acne by increasing sebum production or promoting inflammation [4]. These include:
- Genetics
- Hormonal fluctuations
- Diet
- Stress
- Certain medications
Avoidable risk factors include high glycemic diets, smoking, and harsh skincare products.

Acne Presentation: Recognizing the Patterns
Acne often emerges during puberty, coinciding with increased androgen levels.
- Younger teenagers frequently experience milder, non-inflammatory acne, mainly composed of open and closed comedones (blackheads and whiteheads).
- Older teenagers and adults are more prone to developing inflammatory acne lesions like papules, pustules, nodules, and cysts as sebum production increases.
Traditional Chinese medicine describes different acne “patterns” [5], including:
- Wind-Heat Type: Characterized by sudden onset and red papules.
- Damp-Heat Type: Associated with oily skin and nodules/cysts.
- Phlegm-Static Blood Type: Manifests as firm nodules.
- Disharmony of Vessels Type: Presents with purplish cysts on the neck and chest.
The development of inflammatory lesions is closely linked to changes in the skin’s microbiome, barrier function, and immune responses [3].
The Significant Psychological Impact of Acne
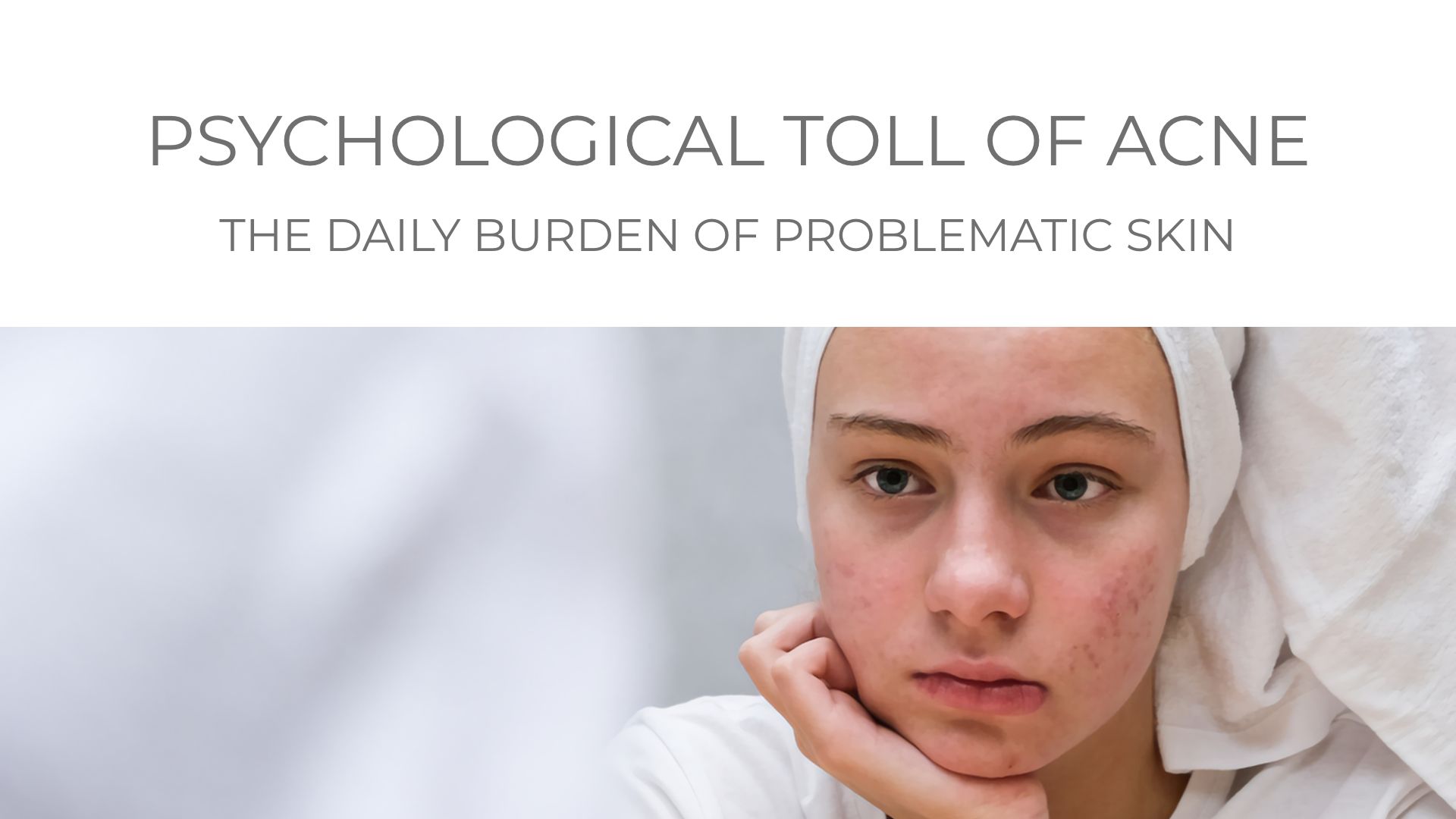
Beyond the physical symptoms, acne often carries a substantial psychological burden. Research consistently shows higher rates of:
- Anxiety
- Depression
- Psychological stress
- Social isolation
- Suicidal thoughts
among individuals with acne [6].
Key points about the psychological effects of acne:
- Depression risk: Individuals with acne are 2-3 times more likely to experience clinical depression.
- Social and self-esteem impacts: Acne negatively affects social interactions, self-esteem, and overall quality of life.
- Severity correlation: Psychological distress often increases with acne severity.
- Gender differences: Females may experience greater psychological effects than males.
- Scarring: Acne scarring can worsen psychological symptoms.
Addressing the psychological aspects of acne is crucial in treatment plans. Counseling, stress management techniques, and antidepressant medications can be beneficial additions to dermatological treatments.

Acne Diagnosis and Diverse Treatment Options
Acne diagnosis is typically made through a review of your medical history and a physical examination [7]. Treatment strategies depend on the severity of acne:
- Mild acne: Often treated with topical medications.
- Moderate acne: May require oral antibiotics.
- Severe acne: Might necessitate stronger oral medications or other aggressive interventions [8].
Treatment adherence is essential for achieving positive results [9].
Newer acne therapies are continually emerging, including clascoterone, sarecycline, trifarotene, and advanced formulations of tretinoin and tazarotene. Medicinal plant extracts with antibacterial properties against acne-causing bacteria are also being explored [10].

Given the multifaceted nature of acne, various treatment approaches are available. Here’s a summary of common treatments:
- Topical Retinoids: Often the first-line treatment, retinoids like tretinoin, adapalene, and tazarotene work by unclogging pores and reducing inflammation by influencing cell differentiation and cytokine production.
- Benzoyl Peroxide: This antibacterial and anti-inflammatory agent targets Cutibacterium acnes. It’s frequently used with retinoids but can cause dryness and irritation.
- Topical Antibiotics: Clindamycin and erythromycin are used to reduce bacteria, but sparingly to prevent antibiotic resistance.
- Oral Antibiotics: Tetracyclines, such as doxycycline and minocycline, are often prescribed for moderate to severe inflammatory acne, typically combined with topical treatments.
- Hormonal Therapies: Oral contraceptives and spironolactone can treat hormonal acne in females by reducing androgen stimulation of sebaceous glands.
- Oral Isotretinoin: The most effective treatment for severe nodulocystic acne. It significantly reduces sebum production but requires careful monitoring due to potential side effects.
- Emerging Therapies: Novel treatments under investigation include topical antiandrogens, photodynamic therapy, laser and light therapies, sonophoresis, and microneedling [11]. Lifestyle adjustments like a low glycemic diet and stress management can also be beneficial.
Matching Treatment to Acne Severity
Acne severity is a key factor in determining the most appropriate treatment. The following table outlines acne severity classifications and corresponding treatment approaches to ensure tailored care:

| Acne Severity | Characteristics | Treatment Implications |
|---|---|---|
| Mild Acne | Mostly comedones with occasional papules/pustules | Often manageable with over-the-counter products and low-strength retinoids. |
| Moderate Acne | More pronounced inflammatory lesions | May require prescription medications to reduce inflammation. |
| Severe Acne | Nodules, cysts, widespread involvement | Typically necessitates more aggressive treatment, like oral isotretinoin and procedures for cysts. |
| Very Severe/Refractory Acne | Severe scarring and/or fistulas | May require intensive therapies, including high-dose isotretinoin and surgical interventions. |

Acne vs. Seborrheic Dermatitis: Distinguishing Key Differences
Seborrheic dermatitis shares some similarities with acne but has crucial distinctions. Unlike acne, seborrheic dermatitis is primarily linked to an overgrowth of Malassezia yeasts [1].
Location Differences:
- Acne: Typically affects the face, chest, and back.
- Seborrheic dermatitis: Commonly impacts the scalp, face, ears, chest, and skin folds.
Cause of Symptoms: The scaling and flaking in seborrheic dermatitis result from inflammation triggered by fungal lipids and metabolic byproducts. The immune system’s response to Malassezia yeast drives the redness and itching.
Shared Factors: Excess sebum production likely contributes to the overgrowth of both Cutibacterium acnes in acne and Malassezia yeast in seborrheic dermatitis. Changes in sebum composition may also play a role. Both conditions can be worsened by psychological stress, suggesting potential shared neuroendocrine pathways [6].
Quick Comparison: Acne vs. Seborrheic Dermatitis
| Characteristic | Acne | Seborrheic Dermatitis |
|---|---|---|
| Primary Locations | Commonly appears on the face, chest, and back. | Occurs in areas with high sebaceous gland activity, such as the scalp, face, and chest. |
| Lesions | Characterized by comedones, papules, and pustules. | Presents as flaking, scaling, and inflammation. |
| Microbiome Involvement | The skin microbiome plays a role, with altered diversity and composition. | Malassezia yeast colonization is a key factor, along with bacterial imbalances. |
| Hormonal Influence | Hormones like androgens contribute to increased oil production. | While hormones may play a role, they are not as central to the condition’s pathogenesis. |
| Psychological Impact | Often linked to anxiety, depression, and stress, with well-documented effects. | Though it can be distressing, psychological impact is less widely documented and discussed in the literature. |

In Conclusion: Managing Acne and Seborrheic Dermatitis
Acne vulgaris is a widespread skin condition with a complex development involving sebum, keratinization, skin bacteria, inflammation, and hormones. Seborrheic dermatitis, while sharing some features, is primarily driven by Malassezia yeast overgrowth.
Treatment for both conditions typically involves topical and oral medications aimed at reducing oil, inflammation, and microbial imbalance. Integrating psychological support and lifestyle adjustments can significantly enhance treatment outcomes. Further research into the skin-hormone interactions in these conditions is needed to develop more targeted and less side-effect-prone treatments.
Key Takeaways:
- Acne vulgaris is highly prevalent, affecting a large majority of adolescents and many adults, and is influenced by sebum, Cutibacterium acnes, and inflammation.
- Acne significantly impacts mental health, often leading to anxiety and depression, highlighting the importance of comprehensive care.
- Acne treatment is tailored to severity, ranging from topical solutions for mild cases to oral medications and procedures for severe acne.
- Seborrheic dermatitis, while similar to acne, is mainly caused by Malassezia yeast overgrowth and affects different body areas.
- Both acne and seborrheic dermatitis are linked to excess sebum and can be worsened by stress, indicating potential common pathways.
- Acne mainly affects the face, chest, and back with comedones and inflammatory lesions, while seborrheic dermatitis targets sebaceous gland-rich areas with flaking and scaling.
- Hormones are a major factor in acne due to androgen influence, whereas seborrheic dermatitis is less hormonally driven.
- The psychological effects of acne are well-documented, while those of seborrheic dermatitis are less discussed, though both can impact quality of life.

No Comments
Be the first to start a conversation