Seborrheic DermatitisThe Owner’s Manual

+12k User downloads
18.99 Single payment
+500 Pages
Everything you should know about the condition and its treatment
- My personal experience with the condition
- What the medical world knows about it and its cause
- How its diagnosed and similar conditions you need to be aware of
- A detailed review of more than a dozen proven treatments
- The importance of digestion, immune function, and the nervous system in skin disease
- A proposed systemic approach to long term relief
Purchase downloads
Both versions | Liberal return policy

Reader Reviews
FAQ
Can I download to my Kindle?
A MOBI version of the book is included. This file can be emailed directly to your dedicated Kindle email for reading on your device.
Where to buy a physical copy?
As the book continues to receive updates, it is only available in digital format for the time being.
Ask a Question 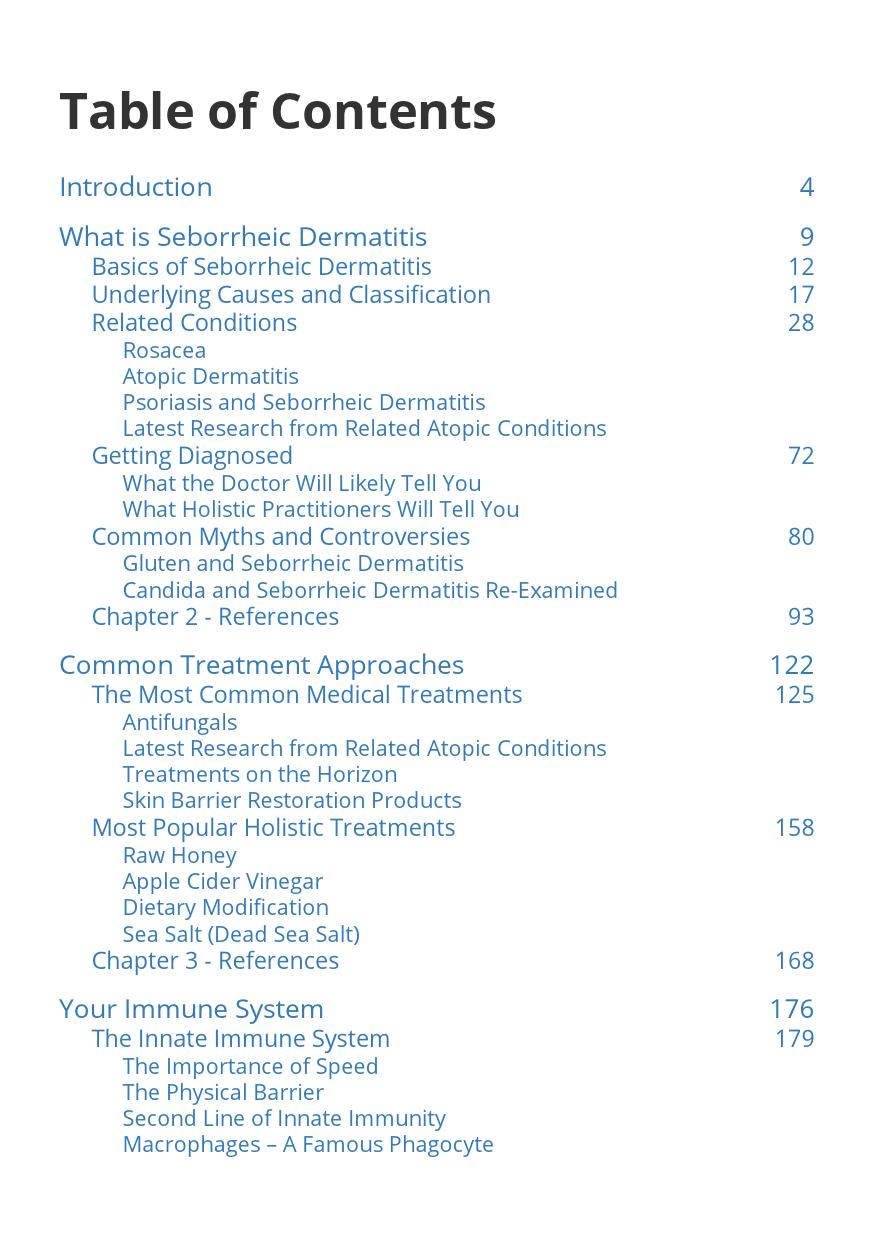
Kerina –
I briefly read the ebook on seborrheic dermatitis as I have 2 young children makes a little difficult to get through everything lol I think it was very informative! I have had seborrheic dermatitis for almost 3 years now. It appeared about 2 months after I gave birth to my daughter so I had a feeling it had to do with drastic change in hormones. During my pregnancy with my son it got a little better and then got worse after delivery.. Since then I’ve have been trying to take a natural approach as I am breast feeding my son Dr’s have prescribed steroid creams. So far I’ve tried ACV and it help the first few days but drastically dried out my skin. I am now using therapeutic grade essential oils and have seen significant change! I just received biom8 conditioning oil in hopes that will help rid this dermatitis! Thank you for devoting your time to share this information with others such as myself! It is greatly appriciated. Great job!
Dora –
excellent